News • Dose reduction
Increasing precision for radiotherapy
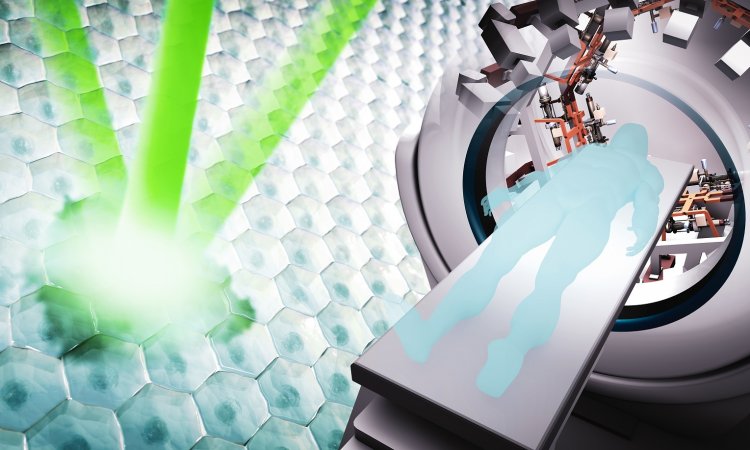
A new way of concentrating radiotherapy dose in tumours, while minimising damage to healthy cells, has been proposed in research led by scientists at the University of Strathclyde.

The study proposes that focusing high-energy particle beams on a small spot deep inside the body could potentially enable clinicians to target cancerous tumours precisely, while reducing the dose to surrounding tissue. External beam radiotherapy involves treating patients with either high energy X-rays or particle beams. Tumour cells are killed by the radiation, which is usually administered in multiple fractions, which are applied daily over several weeks. The main goal is to kill tumour cells using beams of radiation while minimising damage to healthy cells. The study has been published in the Nature Research journal Scientific Reports.
In a similar way to a magnifying glass focusing the sun's rays to a small spot, we propose to focus a particle beam to a small spot using a magnetic lens to ablate the tumour
Dino Jaroszynski
Professor Dino Jaroszynski, who leads the project, said: "Around half of the population will suffer from cancer at some time in their lives. Of these people, half will be treated using radiotherapy or a combination of radiotherapy and chemotherapy. One of the challenges in radiotherapy is to deposit a high radiation dose in a way that the dose fully ‘conforms' to the tumour, to ensure that all cancerous cells are killed, while preventing damage to healthy cells. Our study shows that we can very simply focus radiation onto a tumour to irradiate it while reducing the dose in surrounding healthy tissue. In a similar way to a magnifying glass focusing the sun's rays to a small spot, we propose to focus a particle beam to a small spot using a magnetic lens to ablate the tumour."
Common forms of radiation currently used in radiotherapy include X-rays produced by electron beams from ‘medical' linear accelerators, or linacs, that generate a type of radiation known as bremsstrahlung X-rays, which then target the tumour. These relatively low energy electron beams from the linac can also be used directly to irradiate tumours but they do not penetrate deeply into the body and therefore are not commonly used.
One of the disadvantages of using X-rays in radiotherapy is that they are absorbed in the body and their effects diminish, resulting in a high entrance dose. Proximal and distal doses - before and after the tumour - can also be as high as, or higher than, the radiation dose in the tumour. To irradiate the tumour precisely with sufficient radiation to kill all tumour cells, the X-ray beam is often rotated while pointing at the tumour from different directions, while the patient remains stationary.
Recommended article
Article • Interdisciplinarity
All for one: a Belgian prostate unit at work
Pathologists, radiologists, urologists and radiotherapy specialists sit at the core of the treatment pathway for the patient, working together as a cohesive unit. In an innovative 2019 ECR session in Vienna, the prostate unit from Ghent University Hospital in Belgium outlined how the team works to deliver the best clinical outcome for patients.
An effective radiotherapy modality uses heavier particles such as protons and ions. These have the advantage of radiation doses that can be confined to a small region called the "Bragg peak". Proton radiotherapy facilities are available but are very expensive.
Dr Enrico Brunetti, a Research Fellow in Strathclyde's Department of Physics involved in the project, said: "This work presents a comprehensive numerical study of fundamental issues encountered in cancer treatment with very high energy electrons for a wide range of geometries. Results suggest that technology and beam transport systems routinely employed in high-energy particle accelerators could find direct application in this field, expanding the range of tools available for radiotherapy."
Karolina Kokurewicz, a Strathclyde PhD student working on the project, said: "Electrons, much like protons, have properties specific to particles. The significantly smaller electron mass, however, must be compensated for by increasing their energy and therefore inertia to achieve an effect similar to high mass particles. We push the envelope to fully investigate the potential advantages of very high energy electrons (VHEEs) in radiotherapy. In our studies, we show that a VHEE beam, when focused, can be easily controlled to target precisely tumours similar to beam scanning modalities. The net effect is a greatly enhanced dose profile that conforms closely to the target volumes and potentially provides better tumour control. It is a first step to realise the real potential of VHEEs."
Professor Jaroszynski said: "We are setting up a new medical beamline at the Scottish Centre for the Application of Plasma-based Accelerator (SCAPA) at Strathclyde, to use laser-produced high energy electron accelerators to investigate the ideas published in our paper. These ultra-compact laser-wakefield accelerators are only millimetres long and can be easily focused; most of the space is taken up by the power supply, which is the laser. This is a very exciting new project that has potential to eventually transform radiotherapy by reducing its cost, while improving its effectiveness."
Source: University of Strathclyde
29.07.2019