News • Cancer treatment
Immunotherapy approach 'points' killer cells towards tumours
Immunotherapy, a therapeutic strategy aimed at increasing the activity of the immune system in order to recognize and destroy cancer cells, has revolutionised cancer treatment over the past decade.
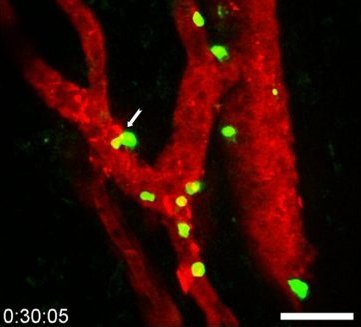
© Elisabeth Bellard and Jean-Philippe Girard – IPBS (CNRS/UT3 Paul Sabatier)
A better understanding of how this therapeutic approach works, and more particularly how killer lymphocytes access tumours during immunotherapy, could improve the efficacy of the treatments. The team of Jean-Philippe Girard, Inserm Research Director at the Institute of Pharmacology and Structural Biology (French National Center for Scientific Research [CNRS]/Université Toulouse III – Paul Sabatier), in collaboration with Gustave Roussy, has recently discovered the essential role played in this process by specific blood vessels known as tumour-associated HEVs. For the first time, the scientists were able to film the lymphocytes infiltrating the walls of the HEV vessels to enter the tumours. What is more, the researchers have shown in animal models that increasing the proportion of HEV vessels in a tumour improves the efficacy of the immunotherapy and leads to the eradication of the tumours. Finally, they found that the likelihood of recovery of patients with metastatic melanoma (skin cancer) and treated with immunotherapy is increased when a large number of HEV vessels are present in tumours. The findings of this study have been published in the journal Cancer Cell.
Immunotherapy with therapeutic antibodies represents a real revolution in cancer treatment. In particular, it is used to cure certain patients with metastatic melanoma, who would previously not have survived. Unfortunately, immunotherapy is not effective in all patients or on all cancers. A better understanding of the mechanism of action of the treatment could improve it and make it effective in a larger number of patients. Killer lymphocytes – white cells present in the blood – are capable of eradicating cancer cells. It is essential that many of these killer cells have access to tumours in order to defend the body against cancer. The Toulouse team has lifted the veil on the mechanisms that allow killer lymphocytes to penetrate tumours in order to destroy them – either spontaneously or following immunotherapy with anti-PD-1 plus anti-CTLA-4 antibodies.

© Jean-Philippe Girard – IPBS (CNRS/UT3 Paul Sabatier)
The scientists have discovered that the HEVs, very specific blood vessels known as high endothelial venules, constitute the major gateway of lymphocytes to tumours. Using sophisticated microscopy techniques, the researchers were able to film the passage of lymphocytes from the blood to the tumour in animal models. For the first time, they were able to visualise, directly and in real time, the lymphocytes in the process of infiltrating the walls of the HEV vessels in order to access the cancer cells in the tumour. “We thought that HEV vessels played an important role in the entry of lymphocytes into the tumour, but we were surprised to see that they were virtually the only gateway,” says Jean-Philippe Girard, Inserm Research Director and last author of the study.
Our research could improve immunotherapy treatment in the longer term for patients with metastatic melanoma and other types of solid tumours
Jean-Philippe Girard
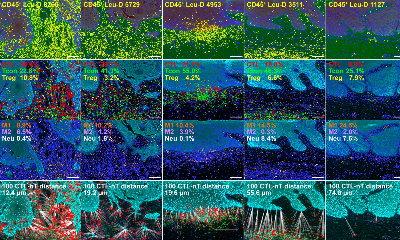
The researchers then observed in their models that the presence of a large number of killer lymphocytes in tumors is associated with the presence of a large number of HEV vessels. What is more, they provided proof of concept that increasing the proportion of HEV vessels in a tumour improves the efficacy of combination anti-PD-1 plus anti-CTLA-4 immunotherapy and leads to tumour eradication.
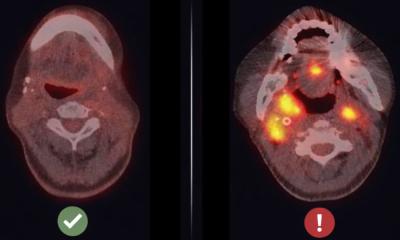
Finally, in collaboration with Caroline Robert’s team at Gustave Roussy, the scientists studied patients with metastatic melanoma. They discovered that the presence of a large number of HEV vessels in tumours is associated with a better response to combination anti-PD-1 plus anti-CTLA-4 immunotherapy.
The next step for the researchers will be to develop treatments to increase the proportion of HEV vessels in tumours, in order to improve the efficacy of immunotherapy, allowing massive recruitment of killer lymphocytes to eradicate cancer cells. “Our research could improve immunotherapy treatment in the longer term for patients with metastatic melanoma and other types of solid tumours. It also has prognostic implications, as clinicians can now look at the HEV vessels to predict a patient’s response to immunotherapy,“ concludes Girard.
Source: Inserm
05.02.2022