Image credit: Radiological Society of North America (RSNA)
News • Breast cancer detection
Decade of DBT: 10-year study shows benefits of tomosynthesis
According to a new 10-year study, screening for breast cancer with digital breast tomosynthesis (DBT) increases cancer detection rates and significantly reduces the rate of advanced cancers compared to conventional 2D digital mammography.
The findings were published in Radiology, a journal of the Radiological Society of North America (RSNA).
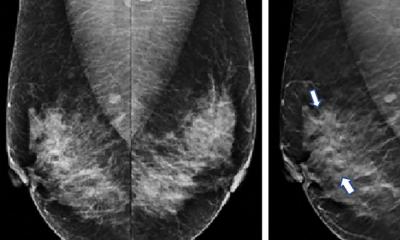
Mammography is considered the gold standard in breast cancer screening for the general population. However, conventional 2D mammography, in which a low-dose X-ray system produces pictures of the inside of the breast from two angles, fails to detect approximately 20% of breast cancers. It is also associated with false-positive results, where an abnormality seen on a screening mammogram turns out not to be cancer after a woman has been recalled for and undergone additional tests.
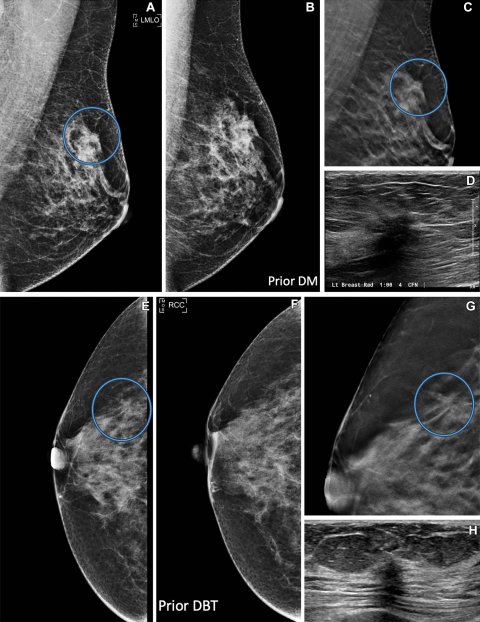
Image credit: Radiological Society of North America (RSNA)
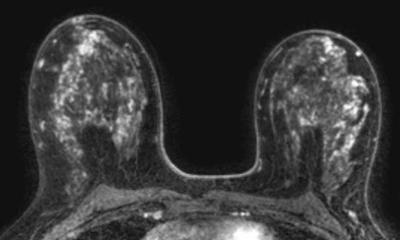
DBT is an advanced form of mammography that reconstructs pictures of the breast taken from different angles into 3D images. Studies have found that DBT has a higher cancer detection rate compared to digital mammography. “This study is the first to compare 10 years of data on breast cancers detected by DBT to digital mammography-detected cancers,” said co-author Jaskirandeep Kaur Grewal, PA-C., previous student at Yale School of Medicine Physician Associate Program.
In the retrospective study, Dr. Philpotts and a team of researchers analyzed consecutive cancer cases detected by screening mammography over 13 years at Yale University/Yale-New Haven Health. The data included 10 years of mammograms performed with DBT, which became the standard at Yale facilities beginning in 2011, and the preceding three years of mammograms performed with digital mammography.
The study cohort included 272,938 screening mammograms, of which 35,544 were performed with digital mammography, and 237,394 were performed with DBT. A total of 1,407 cancers were detected, 142 by mammography and 1,265 by DBT. “Overdiagnosis has been a hot topic in mammography screening. Skeptics of mammography screening believe that the use of DBT results in overdiagnosis,” said first co-author Liane Elizabeth Philpotts, MD, professor of radiology and biomedical imaging at Yale School of Medicine in New Haven, Connecticut. Overdiagnosis means the cancers found are not clinically relevant and may not cause a health concern for the patient if left undetected.
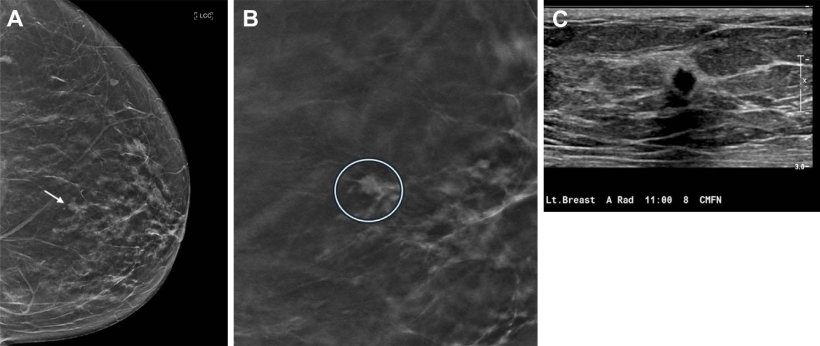
According to Dr. Philpotts, digital mammography and DBT detected various subtypes and grades of tumors at similar rates. The ratio of invasive cancers to ductal carcinoma in situ (DCIS) did not differ significantly between the two modalities. “We found that digital mammography and DBT screening mammography found the same types of cancers, but at different stages,” she said. “DBT found more aggressive cancers at an earlier stage compared to digital mammography.”

Image source: RSNA
DBT had a higher cancer detection rate than mammography (5.3% versus 4.0%) and a lower rate of advanced cancers (32.7% versus 43.6%), indicating that cancers are likely being detected earlier. Cancer detection was improved when women had repeat mammograms with DBT. Most true-positive cancer cases detected by DBT presented as masses, while fewer presented as calcifications and asymmetries.
The recall rate for DBT (7.2%) was significantly lower than for digital mammography (10.6%). “DBT’s lower recall rate, higher cancer detection rate and lower rate of advanced cancers is a win, win, win,” Dr. Philpotts said. “I think this data will contribute to the debate of overdiagnosis by demonstrating that DBT is not over-diagnosing cancers. It’s finding the bad actors earlier.”
Dr. Philpotts said additional studies using long-term data are needed to better understand the role of DBT in screening outcomes. “These findings add to the growing literature regarding cancer detection with DBT and support its use in screening mammography in the United States and globally,” Dr. Philpotts said. “Our results may provide healthcare institutions that have not yet switched from digital mammography to DBT with the data they need to adopt the newer technology.”
Source: Radiological Society of North America
18.09.2024