Article • From generic to personalised, from empirical to evidence-based medicine
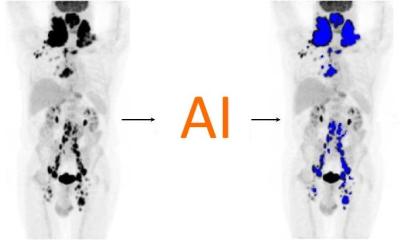
Hopes for hybrid imaging lie in AI
During a European Society of Hybrid, Molecular and Translational Imaging (ESHI) session at ECR 2019, three speakers discussed the role of artificial intelligence (AI) in hybrid imaging.
Report: Mark Nicholls
While AI and machine learning is supporting clinicians using hybrid techniques such as PET/CT, MR/PET, or ultrasound and CT, challenges remain in ‘training the machines’ to add value to radiologists’ and image analyses. To do that, large amounts of data are needed but, to enable proper data mining and machine learning, Osman Ratib, professor at the University of Geneva and Chair of the Division of Medical Imaging at Riviera-Chablais Hospital in Vevey, Switzerland believes the medical world still falls short in providing the necessary amount of data in a well-organised and curated way. He pointed to the need for open research data in an era where medical practice has changed from generic to personalised, from empirical to evidence-based.

Five Big Data challenges were itemised: no common vocabulary in radiologists’ reports; a lack of annotation and mark-up standard; the need for measurement uniformity with multiple image interpretation platforms; the need for public data sets and to create a shared imaging archive; and an ongoing disconnect between DICOM and HL7. ‘We need Big Data archives but it’s difficult to get different centres to contribute to that,’ Ratib pointed out. He also dismissed fears that AI could make radiologists obsolete one day. The discipline needs to embrace the tools as ‘aids and enhancements to human intelligence’ and to help alleviate the global shortage of radiologists by enhancing productivity; improving diagnostic accuracy and delivering fewer misdiagnoses.
Educating the machines remains a leading challenge. The aim is to transfer human knowledge without having to put an algorithm into the machine, Ratib explained, because machines learn to perform image analysis in a ‘supervised’ and ‘unsupervised’ way. ‘The unsupervised part is when it gets scary because we do not know quite what is in the black box and what the machine is thinking. The challenge of the unsupervised element is trying to work out what we want the machine to do that we are not doing today.’
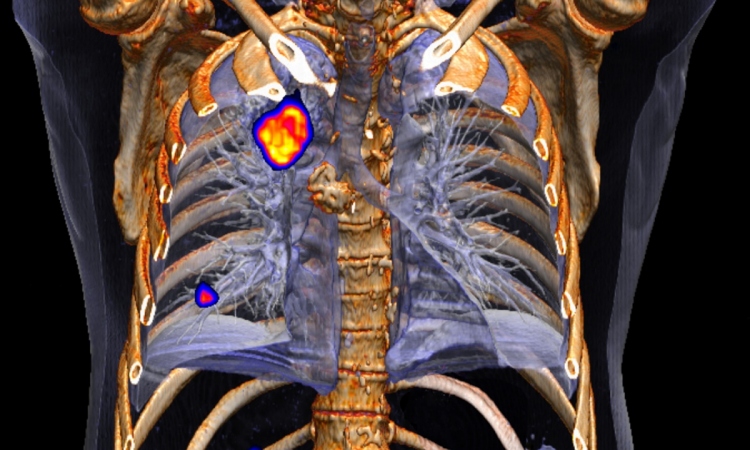
Imaging biomarkers are a major component of Big Data driven medical knowledge and decision-making, the professor concluded and predicted that structured databases of diagnostic imaging will play a major role in the era of personalised medicine with new radiomics features able to provide a significant advance in computer aided diagnosis.
Artificial intelligence, radiomics and holomics

Dr Irène Buvat, from the Service Hospitalier Frederic Joliot in Orsay, France, focused on the role of AI and holomics in predicting what is true from hybrid imaging and non-imaging data. Whilst radiomics is about designing predictive models from image-derived features, using AI to select the best combination of features and create a predictive model, holomics takes this to a new level and is defined as ‘the gathering of genomic, radiomic, proteomic, clinical, immunohistochemical and many more data, and their integration in predictive or prognostic models’.
Buvat: ‘AI is needed because the human mind cannot comprehend this amount of data, but radiomics in itself is not likely to be sufficient; we should also use clinical data, genetic data, pathological slides and blood samples in addition to imaging.’ Although hybrid modalities can deliver the data, there are challenges to radiomics and holomics on model design and interpretation and how a centre applies its model to data from other centres.
Radiomics plus prediction modelling

Dr Antoine Leimgruber, head of Nuclear Medicine and Oncology at Riviera-Chablais Hospital in Vevey, Switzerland, discussed ‘radiomics+: prediction modelling using convergent data’. He maintained that radiologists have to adapt to be part of a rapidly moving medical arena, describing artificial intelligence as ‘a wonderful asset’ for the medical imaging and hybrid imaging community from the perspective of personalised medicine. Radiologists need to harness that to become relevant players in this new field rather than being side-lined.
‘Medical fields are evolving quickly and the medical imaging community needs to respond,’ he underlined. ‘There are new challenges to imagery, with diagnostic tests such as liquid biopsy, but we can respond by building our expertise; we need to be relevant and give relevant advice to clinicians but also by developing techniques. Through radiomics, radiologists can not only increase the amount of data provided to clinicians but can also ‘join the data stream’.
Profiles:
Osman Ratib is professor at the University of Geneva and Chair of the Division of Medical Imaging at Riviera-Chablais Hospital in Vevey, Switzerland
Dr Irène Buvat works at Service Hospitalier Frederic Joliot in Orsay, France
Dr Antoine Leimgruber is head of Nuclear Medicine and Oncology at Riviera-Chablais Hospital in Vevey, Switzerland
28.06.2019