Drawing radiology and nuclear medicine together
‘Let’s work as a team!’
Dr Gerald Antoch, professor of radiology and chairman of the department of diagnostic and interventional radiology at Düsseldorf University Hospital and active member of several scientific societies, delivered the prestigious Wilhelm Conrad Röntgen Honorary Lecture at ECR 2015 on ‘Hybrid imaging: Let the two worlds of radiology and nuclear medicine come together’.
Report: Marcel Rasch

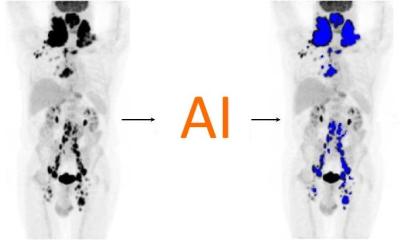
‘A hybrid in medicine has nothing to do with hybrid cars, hybrid bicycles or hybrid golf clubs,’ Professor Antoch emphasised by way of introduction. ‘It is the combination of two imaging modalities, such as PET/CT or PET/MRI, adding that a good imaging system is basically nothing more than a good computer. ‘PET/CT technology, developed to show tumours and metastases that went undetected before, has seen many enhancements since the first system was installed in 2001. However, while in the early days clinicians would say “PET is easy: where it’s light, it’s bad”, today we know that it is not that easy.’
Read image data accurately
The best technology is useless if not supported by people who can read – interpret – the images generated by the technology. ‘You need as much morphology as you can get, but you also need the expertise to read these images,’ Antoch stressed.
‘This expertise has to be available not only for the morphological but also the functional side,’ he added, to avoid misinterpreting findings in different images, because ‘accurate hybrid imaging is a question of knowledge’.
The term ‘Theranostics’ describes the combination of therapy and diagnostics, which requires accurate hybrid interpretation by specialists as a basis.
New standards and comprehensive training
For ‘Theranostics’ to be implemented properly, Dr Antoch said, it must be clear who is responsible for scans and who provides them but, even more importantly, ‘who reads and interprets hybrid F-FDG PET studies’. Often, today, two specialists – a radiologist and a nuclear medicine physician – cooperate on each scan and to ensure that the images were read correctly and to avoid misinterpretation.
‘We need to adapt the workflow to real life,’ Antoch said – with ‘real life’, meaning ‘limited resources’. He proposes the implementation of new training programmes where nuclear medicine specialists familiarise themselves with necessary radiology knowledge and vice versa, depending on the local or country-specific regulations.
What we need for the future
Antoch’s vision for the future is very clear: ‘We must move from separate departments towards one imaging centre. We need new training programmes, a flat organisation, interlinked reimbursements and no turf battles. Let’s work as a team.’
24.06.2015