Article • AI and DL to drive precision medicine
Diving into medical big data
Big data is transforming diagnosis and medical care, but the critical challenge remains over how to equally apply the benefits it delivers across real-world clinical settings. Industry expert Benoît Macq recognises that high quality data can be harvested from major university hospitals and academic centres but is convinced that the true value will emerge when it is accessible in a relevant way to clinicians and patients in smaller hospitals too.
Report: Mark Nicholls

Prof Macq will outline this aspiration, and the value of big data, during his presentation “How to dive into the large-scale dataset?” to the EuroMedLab conference in Munich from April 10-14.
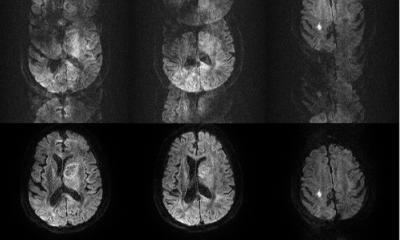
The expert, who leads the PiLAB research team from the Institute of Information and Communication Technologies, Electronics and Applied Mathematics (ICTEAM) at the Université Catholique de Louvain in Belgium, explained that large-scale data sets can create predictors for diagnosis, treatment planning, and drug use, by harnessing Artificial Intelligence (AI) and Deep Learning (DL) technologies to acquire and analyse data to realise these goals.
However, what is key is that there is no centralised point of the data, but a system of “federated learning” where the DL model accesses a range of data silos in different hospitals. This brings data together to create a distributed big data set, but with each institution retaining control of its data from a regulatory, cybersecurity and patient privacy perspective.
Coalitional learning

From this concept of federated learning, which groups organisations together, the drive is to move to the next step of coalitional learning between different institutions ‘to feed the new predictors, the new diagnosis and the new biomarkers.’ With a challenge lying in the varying data quality, annotation, clinical decision making and diagnosis, the move from federated learning to coalitional learning will help provide cross control of data quality, he said. That will remove the variability in data and ‘align human judgement across a coalition’ in sharing data, procedural approaches, and joint strategy on the use of the data.
A shift to coalitional learning increases the quality of the data, ensures validated expertise, and increases accuracy, said Professor Macq, who already applied this together with his team in areas such as proton therapy treatment planning and early detection of breast cancer. His presentation at EuroMedLab will look at managing the process in a decentralised way, and ways to align coalition partners to construct those predictive models for diagnosis, screening, treatment planning, follow up, biomarker design and drug proposition.
As an engineer, rather than a clinician, he emphasised the importance of ‘diving into the data’ from different places and making sense of it and being relevant to the patient. ‘We want to have a convergence with a coalitional learning system where the data acquisition and the predictive model is increasing thanks to the contribution of the different institutions,’ said Professor Macq. He further underlined the importance of different types and sizes of institutions working together, as well as engineers collaborating with clinicians and data scientists, in constructing a DL model that is applicable and relevant to all clinical institutions and their patients.
Accessibility is our goal, and to increase the quality of treatment because it will be more personalised and delivered earlier with better diagnosis and better screening
Benoît Macq
The benefit is to create precision medicine to deliver better diagnosis and patient care, but also facilitate improved natural medicine. ‘The idea is to better understand diseases by trying to find causal relationships between DNA, RNA proteins and metabolics, and between different levels in the biology continuum to augment medicine,’ he said.
He believes precision medicine will lower the costs as screening will be more efficient and treatment more precise and personalised. ‘Accessibility is our goal,’ he said, ‘and to increase the quality of treatment because it will be more personalised and delivered earlier with better diagnosis and better screening.’ This, he hopes, will create a new democracy to the use of the data so patients – whether at a university hospital or local hospital – will benefit equally.
*The “Artificial intelligence, data science and laboratory medicine: crossed destinies” Symposium 6 on April 11 at 2-4pm, will also feature the presentations “The AI data wave, seizing opportunities” and “What are the keys for Europe as a space for data and AI?”
Profile:
Professor Benoît Macq leads PiLAB, a research team from the Institute of Information and Communication Technologies, Electronics and Applied Mathematics (ICTEAM) at the Université Catholique de Louvain in Belgium, where around 30 researchers focus on three main research topics of: Signal & Pixels, Medical Imaging, and Interaction. The co-founder of 11 spin-off companies, he is a Fellow Member of the IEEE (The Institute of Electrical and Electronics Engineers) and a Member of the Royal Academy of Science of Belgium.
07.04.2022