Helical tomotherapy
By Rudolf Schwarz and Andreas Krüll, of the Section of Radiation Oncology Department, Ambulanzzentrum GmbH of the University Medical Center Hamburg-Eppendorf

Designed in the 1990s, the TomoTherapy HiArt treatment system looks like a CT scanner, allowing efficient 3-D-CT imaging to be used to ensure daily treatment accuracy for all patients (Fig. 1). It was designed to combine industry standard imaging and helical radiation delivery (Fig. 2). The accelerator, with an energy of six Megavolts in the gantry, is used for CT scanning and irradiation. It delivers intensity modulated radiotherapy (IMRT) that uses tens of thousands of narrow beamlets, producing the most precise conformal radiotherapy available. HiArt delivers radiation from all angles around the patients. The beam is rotated around the body, while the treatment couch simultaneously moves into the machine. The system ensures accurate delivery of precise helical IMRT plans via 3-D image-guided radiotherapy (IGRT), based on daily pre-treatment megavoltage CTs in treatment position for higher accuracy and precision. Necessary adjustments in patient positioning can easily be made using registered planning and daily CT images for references (Fig. 3).
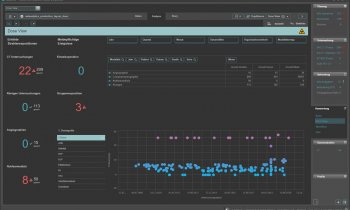
With every treatment fraction, one can see where the anatomy is, compared with where it should be. An overlay of planned dose offers further assurance that the prescription dose level will cover targeted anatomy. Imaging dose with 1-3cGy is consistently low. The system allows for organ movements. Radiation exposure to healthy tissue and organs is minimised. The system integrates tools for optimised, individualised treatment planning, quality assurance, imaging technology, helical IMRT, recording and verification. Delivery Quality Assurance (DQA) is integrated in the planning software, allowing seamless calculation of the dose with the patient’s plan applied to a phantom.
The DQA plan can be selected and delivered from the Operator Station, and compared with point dose and planar film dose measurements. This ensures the prescription will be carried out according to plan.
On average, the full procedure takes about 20 minutes from patients’ arrival in the treatment room until they leave. This includes about five minutes for performance of the daily CT and another five to ten minutes for treatment delivery.
The TomoTherapy HiArt-System was installed at our institution in autumn 2006, and up to December 2007, we had irradiated over 120 patients. Comparison of treatment planning showed that helical tomotherapy brings better dose conformality to the tumour and better sparing of normal tissues than 3-D-conformal radiotherapy and intensity-modulated radiotherapy with the step-and-shoot technique.
Many patients with tumours such head-and-neck, brain, upper abdomen, and prostate cancer, benefit from tomotherapy.
It can be used to re-treat patients who had been irradiated and have a local recurrence. It can be dangerous to re-irradiate, because one can risk complications. So it is important to reduce doses to critical, pre-irradiated structures. Tomotherapy can offer this.
Helical tomotherapy can be done for curative as well as in palliative purposes.
Dose escalation over 80 Gy is essential for the primary treatment of prostate cancer. The limiting factor for this dose escalation can be proctitis. Tomotherapy is a safe tool to reduce the rectal dose and minimise the incidence of proctitis. The higher accuracy and precision brings further benefit by reducing the security margins around the targets. Integration of simultaneous boost with higher doses per fraction presents another treatment option (Fig. 4).
The Tomotherapy system allows delivery of a conformal dose or multiple dose levels to complex targets in the head and neck (Fig. 5). With cancers of the tongue, throat, and larynx, often all the lymph nodes must be irradiated, along with the primary tumour. This usually results in permanent damage to the salivary glands with a life-long dry mouth — xerostomia. With tomotherapy doses to radiosensitive structures (e.g. spinal and parotid glands) can be kept low.
Brain tumours: Tomotherapy can treat multiple tumours, such as brain metastases and large or complex shaped primary brain tumours. For brain metastases it is possible to treat the whole brain to a moderate dose and to escalate the dose to metastases by integration of a boost at the time. Another option is to irradiate recurrent brain metastases after previous whole brain irradiation. Tomotherapy brings substantial benefit for the treatment of the neurocranium and the neuroaxis in one treatment plan and process (Fig. 6).
Tomotherapy in a stereotactic mode can also treat lung cancer. Smaller tumours can be irradiated with hypofractionation at the same time, with low doses to the spinal cord and the lung.
Multiple targets especially multiple metastases can be irradiated simultaneously in one treatment plan.
It is important to evaluate every patient’s cancer to determine which form of radiation therapy is appropriate. 3-D-conformal radiotherapy, IMRT with step-and-shoot or dynamic leaf or stereotactic radiotherapy, are other methods of irradiation and can be beneficial for special cases.
01.03.2008