© American Heart Association
News • From the heart to the brain
Early onset of coronary heart disease increases dementia risk
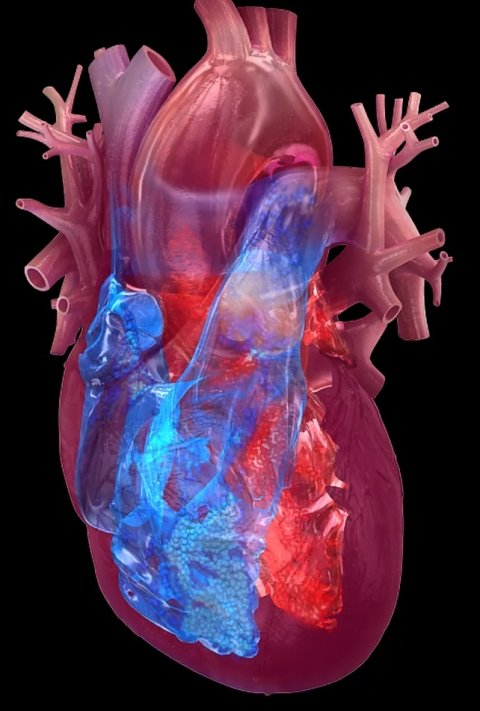
Adults diagnosed with coronary heart disease, especially before the age of 45, may be at increased risk of developing dementia, Alzheimer’s disease and vascular dementia later in life, according to new research.
The work was published in the Journal of the American Heart Association, an open access, peer-reviewed journal of the American Heart Association.
“Coronary heart disease has previously been associated with dementia risk in older adults, however, this is believed to be the first large-scale study examining whether the age of coronary heart disease onset may impact the risk of developing dementia later in life,” said Fanfan Zheng, Ph.D., senior study author and researcher in the School of Nursing at the Chinese Academy of Medical Sciences & Peking Union Medical College in Beijing, China.
What surprised us most was the linear relationship between age of coronary heart disease onset and dementia. This shows the huge detrimental influence of premature coronary heart disease on brain health
Fanfan Zheng
“In previous research, we found that adults experienced accelerated cognitive decline after new diagnoses of coronary heart disease,” she said.
The researchers assessed the potential relationship between age at coronary heart disease onset and the development of dementia by analyzing health data from the UK Biobank.
The analysis found:
- Among the 432,667 participants in the study, there were 5,876 cases of dementia, 2,540 cases of Alzheimer’s disease and 1,220 cases of vascular dementia that occurred over an average of 13 years of follow-up.
- Compared with participants who did not have coronary heart disease, participants with coronary heart disease had higher risks of developing dementia from any cause, Alzheimer’s disease and vascular dementia.
- After adjusting the analysis for demographic and lifestyle factors, participants with coronary heart disease had a 36% increased risk of developing dementia, a 13% increased risk of developing Alzheimer’s and a 78% greater risk of developing vascular dementia.
- Earlier coronary heart disease-onset was associated with a 25% increased risk of dementia, a 29% increased risk of Alzheimer’s disease and a 22% increased risk of vascular dementia.
- The risk of dementia rose in direct proportion to the younger age of coronary heart disease onset (per 10-year decrease in age).
- Participants diagnosed with coronary heart disease before age 45 had a significantly increased risk of developing dementia compared to their counterparts who did not have coronary heart disease.
“What surprised us most was the linear relationship between age of coronary heart disease onset and dementia. This shows the huge detrimental influence of premature coronary heart disease on brain health,” Zheng said. “As more people live longer and are diagnosed with coronary heart disease at a younger age, it’s likely there will be a large increase in the number of people living with dementia in years to come. Health care professionals should be aware of individuals diagnosed with coronary heart disease at a young age. The next step is to determine whether modifying cardiovascular risk early in life will promote better brain health later in life.”
© American Heart Association
Study details and background:
- The UK Biobank is a large, biomedical database and research resource with health records of about 500,000 adults — enrolled from 2006 until 2010 — who live in the U.K and received health care through the U.K.’s National Health Service. The researchers accessed the data in May 2022 and analyzed health records through October to December 2022.
- The researchers analyzed health records for a total of 432,667 adults (average age of 57 years when they became participants in the UK Biobank; 54.6% were female); 11.7% — 50,685 adults — had coronary heart disease at time of enrollment and through the follow-up period. 240 adults who had coronary heart disease were excluded due to missing data about the age at which they were diagnosed with CHD.
- The researchers adjusted the analysis for demographic factors including age, sex, race and education. They also adjusted for lifestyle factors, including smoking status, alcohol consumption and whether participants engaged in moderate or vigorous exercise for over 10 minutes at least twice per week. Health factors considered included baseline body mass index; levels of low-density lipoprotein cholesterol; hypertension status; diabetes status; use of statins; and if they were a carrier for the APOE4 gene, which increases an individual’s risk of developing Alzheimer’s.
- Data on age of coronary heart disease onset and subsequent incident dementia were collected over an average of 13 years of follow-up.
- The researchers controlled for confounding bias, which suggests associations where they may not exist. They then evaluated the association between coronary artery disease onset in different age groups and the development of dementia. 50,445 of the participants with coronary heart disease were divided into three groups based on age of heart disease onset—before age 45; 45 to 59; and 60 and older—and then matched to counterparts who did not have coronary heart disease to gauge the possible relationship between coronary heart disease and dementia.
According to the American Heart Association’s 2023 Statistical Update, coronary heart disease caused 382,820 deaths in 2020. The estimated rate of dementia (alone, not including Alzheimer’s) in U.S. adults, 65 years of age and older, was 10.5% in 2012, with a rate of 7.3% in males and 12.9% in females, according to the Aging, Demographics and Memory Study, which is a supplemental study of the long-running Health and Retirement Study in the U.S.
The study’s limitations included that it is an observational study, meaning the findings do not confirm cause and effect, and that more than 94% of the study population from the UK Biobank self-identified as white, meaning the findings may not be generalizable to people of other races or ethnicities.
Source: American Heart Association
29.11.2023