Determining the site of deep brain implants
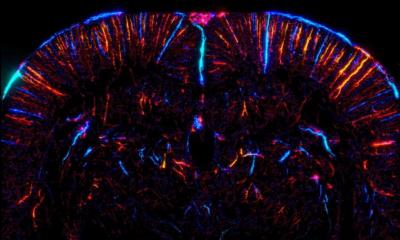
Uncontrollable convulsions, tremor or spasms can considerably impair the lives of neurodegenerative disease patients. Deep brain stimulation (DBS) – for which tiny electrodes are implanted in the brain to stimulate the target areas continuously with electrical impulses – can significantly reduce the movement disorder.

Whilst, due to its enhanced image quality, magnetic resonance imaging (MRI) is the ‘gold standard’ to determine the position of the implants, state-of-the-art ultrasound is increasingly the modality of choice to control the position of the electrodes accurately and in a stress-free way. This has many advantages for patients who, due to the disorder, find it difficult to lie still, explains Professor Uwe Walter, Deputy Director of the Clinic and Polyclinic for Neurology at the University Hospital Rostock, Germany. During the WFUMB Congress he will present* exciting pioneering work on the use of transcranial ultrasound for deep brain stimulation (DBS)
Today, DBS is primarily used in patients with Parkinson’s disease, idiopathic dystonia and tremor. Further indications currently being researched include Tourette’s syndrome, certain psychological disorders and in some cases epilepsy. Intra-operative and post-operative imaging is an important tool to determine and control the location of the electrodes in the brain. Particularly, when a DBS patient’s condition worsens over time, for example due to accident-related head trauma, the position of the electrodes must be verified.
As few as fifteen years ago, controlling the electrode position with ultrasound was inconceivable because b-mode transcranial sonography (TCS) did not clearly identify small echogenic structures in the deep brain.
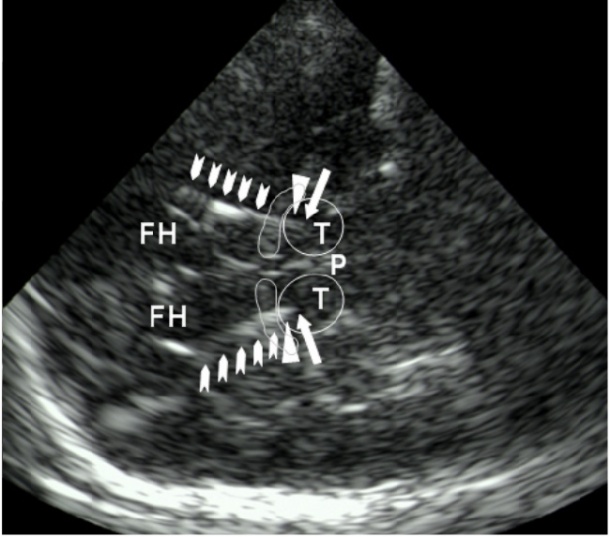
However, today both image quality and resolution have vastly improved and in 2008 Professor Walter and team could already show in a study (pub: NeuroImage) that ultrasound has caught up with MRI. ‘Modern ultrasound technology displays microelectrodes that are placed in a distance of one to two millimetres to each other. Therefore we in Rostock use sonography as first-choice imaging modality when we need to check the position of the leads postoperatively. Secondary CT imaging has always confirmed the ultrasound findings’, the neurologist points out.
Walter’s follow-up study, published in the current issue of Ultrasound in Medicine and Biology and which he will present at the WFUMB Congress, indicates the transcranial sonographic localisation of DBS electrodes predicts the clinical outcome after twelve months. Furthermore, the study suggests that MRI and ultrasound measurements correlate well and that TCS impacts neither on lead temperature nor electrical parameters of the DBS device nor the patient’s clinical state. Thus the study may well promote widespread clinical use of TCS in this field.
Additionally, postoperative location control of DBS electrodes with ultrasound offers further advantages over other imaging modalities. Patients with motion disorders often find it difficult to lie still during a lengthy MRI procedure. Ultrasound offers instantaneous images and uncontrolled head movements, as they occur in dystonia or Parkinson’s patients, can be easily corrected with the hand-held transducer.
Professor Walter continued his ground-breaking research and, with his team in 2009, became the first to publish results, on intra-operative TCS monitoring of DBS electrode position in the basal ganglia through intact skull, in Movement Disorders.
The technique
The neurosurgeon drills small holes in the skull to insert the electrodes into the target areas in the brain, while an ultrasound expert sonographically examines the patient’s head. The latter follows the navigation of the implant through the brain tissue onscreen and, to avoid injuries, tells the surgeon precisely where the electrode needs to move in relation to surrounding vessels. ‘This technique has been available for quite some time but is rarely used because transcranial sonography is primarily performed by neurologists and rarely by neurosurgeons,’ Professor Walter explains.
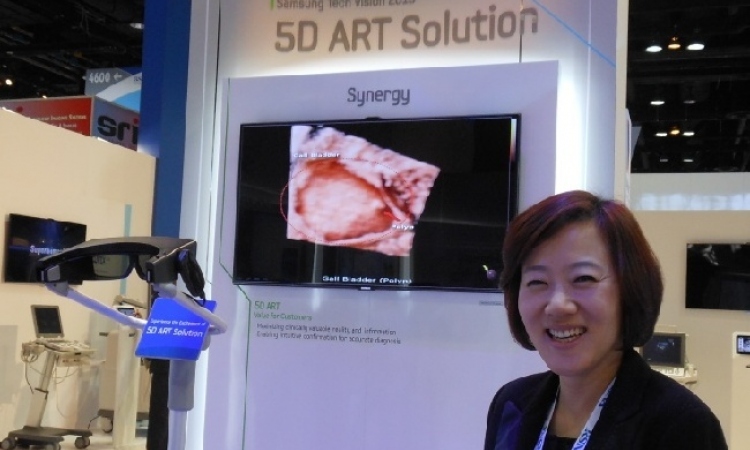
Intra-operative TCS is still facing one obstacle: It does not allow clear identification of certain areas in the basal ganglia and therefore is not suited for precise targeting of the implants. However, Professor Walter is convinced that this obstacle will soon be surmounted. ‘Fusion imaging will be the next major milestone and a quantum leap for sonography in intra-operative image-guided implantation of deep brain electrodes. There are already ultrasound systems offering side by side MRI and ultrasound images to compare and facilitate navigation in the target structures. This technology needs fine-tuning because the patient’s head should be positioned in a certain spatial relationship to the imaging system, but basically it does work.’
For next year Professor Walter is planning a multi-centre study on the use of ultrasound for the post-operative position control of DBS leads, aiming to establish this procedure further, in clinical settings.
International partners from the Czech Republic and the US have already voiced their interest in participating in the study. Hopefully at one of the next WFUMB congresses, we will hear more about this exciting technique.
"Intra and postoperative monitoring of deep brain implants", Sunday, August 28, 09:20-09:45, Hall LM
Uwe Walter
In 1999, Professor Uwe Walter MD trained as a neurology specialist at the Clinic and Polyclinic of Neurology at the University Hospital Rostock, Germany. In 2004 he received the Science Prize of the German Society of Ultrasound in Medicine and, in 2009, was appointed supernumerary professor for neurology at the University of Rostock.
This year he was appointed Deputy Director of the hospital’s Clinic and Polyclinic of Neurology and focuses his research on brain sonography in patients with movement disorders and neurodegenerative diseases, ultrasound diagnostics in neurology (brain, vessels, and nerves) and pathogenesis of stroke-associated pneumonias.
25.08.2011