Determination of angiogenesis with MRI enables timely monitoring of therapy
The suppression of angiogenesis is an established procedure used to make a positive impact on tumour growth and the development of metastases - with varying success.

Whether the therapy is actually successful and the tumour shrinks, or disappears, usually can only be checked about four to six weeks later, during a control examination. The classic parameters currently used in radiology only allow for the assessment of tumour size and volume, which only become visible after a while, or, in the case of stagnation, not at all.
However, the results of a study on the quantitative imaging of angiogenesis through MRI with measurement of the vascular volume fraction promise a significant improvement of oncological therapy monitoring.
Professor Christoph Bremer MD and team at the Institute for Clinical Radiology, at Münster University Hospital (UKM), Germany, has developed this procedure in co-operation with Dr Hannes Dahnke (Philips Research, Hamburg) and is currently working on a clinical translation of the technology. The results, along with a study with optimised measuring techniques for the determination of angiogenesis, are to be presented to specialists at this year’s RSNA. Here, Professor Bremer explains the principle and possibilities of the procedure.
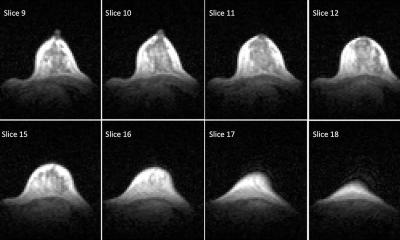
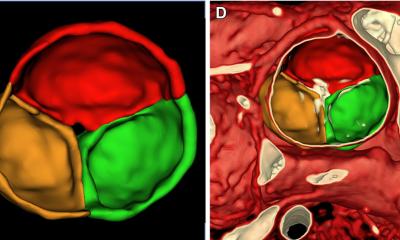
Our objective is to use the method we have developed to determine and measure at a very early stage if and how therapy for the suppression of angiogenesis works. We use iron oxides as contrast media – these remain predominantly in the vessels during measurements and change the MR signal in the respective locations. This change is proportional to the amount of microvessels, i.e. newly formed vessels. This allows us to determine the strength of blood flow in the tumour and therefore gauge how aggressive it is. This process may sound quite banal, but it is highly complex regarding both the contrast medium and imaging technology in the MRI. With normal settings the MRI only delivers anatomical images that allow us to see the tumour, but we need to know how many microvessels are in the tumour.
The significant issue here is sequencing technology, which we have been researching with our partners for many years and which now allows us to achieve stable measurements that, apart from images, also deliver reproducible figures. We use a sophisticated T2/T2 measurement for this, which allows us to compare values at different points in time. To achieve truly valid figures we had to spend considerable time optimising the procedure – but now we are definitely on the right track. Part of these results will be introduced in detail at the RSNA.
We are currently testing the imaging of angiogenesis via MRI on small animals. However, at the same time we are also carrying out the first studies on human patients. We have data on the vascular volume fraction of patients with acute myeloid leukaemia, which help us to further develop the technology for therapy monitoring in humans.
The new procedure could potentially give us an enormous time advantage for therapy management. In theory, depending on therapy, we should be able to monitor success within the first 24 hours from the start of therapy. Experimentally we have been able to produce good results within three to six hours after therapy has begun and were able to retrace a vascular thrombosis.
The determination of angiogenesis is currently not the only option to monitor therapy; there are procedures in molecular imaging using PET and PET-CT that follow a similar objective. However, by comparison, our MR based procedure is less complex and easier for the patient, as there is no exposure to radiation. Additionally, the contrast medium – iron oxide – is fed into the haemoglobin metabolism and therefore does not put a strain on the body. These are competing procedures and the so-called quantitative ‘MRI’ is a promising alternative, which – and these are dreams of the future at this stage
– apart from the measurement of new vessels, also has the potential to show cell movement in the tissue, which can play an important part in both tumours and stem cell transplantation.
30.10.2007