Article • Physics in medical imaging
CT advances: small steps and huge strides
Recent advances in CT have focused mainly on software, yet new technology could push the modality much further, experts showed at ECR 2022.
By Mélisande Rouger

Image source: RSNA
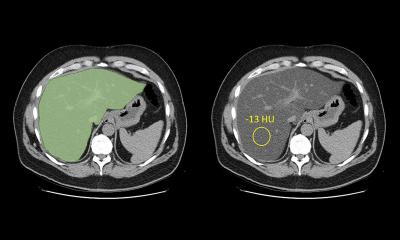
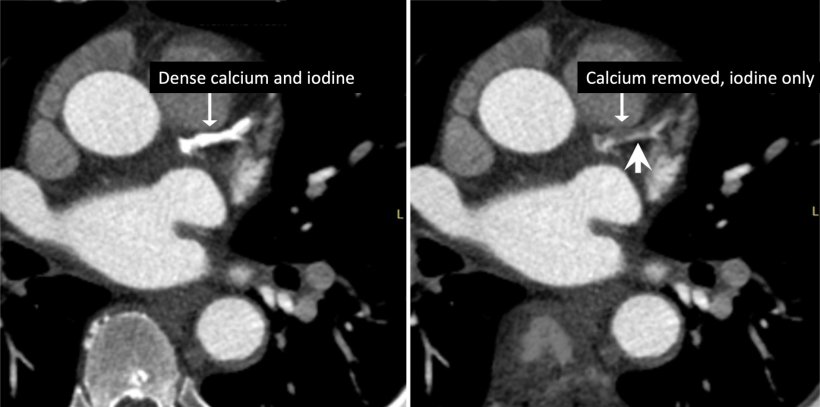
Photon counting is one of the most exciting advances in CT, Cynthia H. McCollough, Director of the CT Clinical Innovation Center and X-ray Imaging Core at Mayo Clinic in Rochester, US, told the audience. ‘It gets rid of the electronic noise streaking artifacts through dense anatomy, where the number of photons is simply so low that the “signal” is primarily from electrical noise, giving equal weight to every photon that is registered,’ she said. ‘This so-called “count weighting” is ‘a major improvement that really boosts the iodine signal in the image for the same amount of injected contrast material compared to non-photon counting detector scanners.’
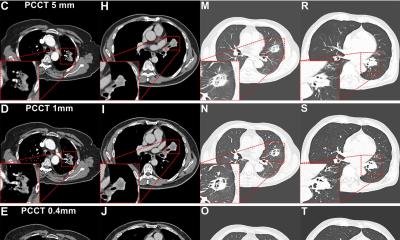
A game changer with photon counting is that the spatial resolution characteristics of the system are fundamentally better, according to McCollough, who has been working with the system for many years. ‘A huge win so far has been in imaging structures,’ she said. ‘Photon counting CT picks up details of the tiniest bone structures such as the inner ear, or hidden fractures, while decreasing radiation dose quite significantly.’

Imaging improvements also concern lung anatomy, while radiation doses can be lowered for chest CTs, for example in children with cystic fibrosis, who usually receive an annual scan for check-up. ‘You see some disease progression on the x-ray, but pretty advanced by the time it shows up,’ McCollough said. ‘We did this very low dose chest CT with the new scanner and paediatric doctors were amazed how much earlier they could see disease patterns compared with an x-ray.’
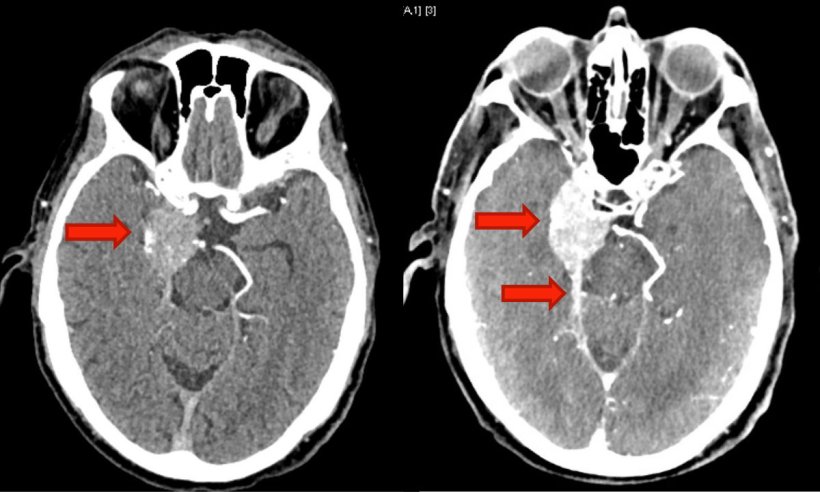
In brain tumour patients, photon counting CT also unveils new findings by measuring the energy of the photons, McCollough explained. ‘It can create new types of images and synthesize an image in which every photon was 45 keV. When you do that, iodine gets super bright, enabling you to see parts of the tumour that were invisible with conventional CT.’
Hardware and software trends

Image source: Radboud UMC
Hardware development has taken a backseat compared with software in recent years, and most efforts have focused on optimizing already existing technology, Mathias Prokop, Head of the Department of Medical Imaging at Radboud University Medical Center in Nijmegen, the Netherlands, said in the following talk.
One such development is the stronger pre-filtering of the x-ray beam using copper, tin and, most recently, silver. ‘This pre-filtering makes the beam harder and ensures that low-energy radiation that usually gets stuck in our patients is now almost completely removed from the x-ray spectrum,’ he said. ‘This reduces radiation dose without impacting image quality.’
The expert also regarded photon counting as ‘a huge stride’ in CT technology, notably for spectral imaging – a promising technique, which is still rarely used in clinical practice. ‘Part of the reason is that special acquisition techniques had to be used and you had to pay a penalty in terms of increased radiation dose,’ Prokop explained. ‘Photon counting solves both issues.’ However, the dual-energy geometry used in the new scanner also generates multiple output datasets that add a layer of complexity – an additional challenge for the clinical high throughput environment in radiology departments. ‘Techniques are needed that make dual-energy information more readily accessible to fit daily practice,’ he said.
Over-reliance on image reconstruction should be avoided
Only if you optimize scan protocols properly on a regular scanner either for optimum resolution or low dose, then a fair comparison can be made with a new scanner with respect to dose and resolution
Mathias Prokop
Lately there has been a substantial improvement in image reconstruction software, especially with model-based iterative and deep learning reconstruction. ‘Deep learning reconstruction provides the best image quality for the lowest possible dose. It’s also comparatively fast,’ Prokop said. The downside with these reconstruction techniques becomes apparent when dose falls below a certain threshold. In these cases, the machine will produce images that look ok, but due to lack of sufficient detector signal, the information is not in the raw data. ‘The likeliest thing will be made up,’ he said. ‘A coronary appears as a coronary and not a coronary with a plaque. A cyst will become either homogenous or heterogeneous depending on chance. Sufficient detector dose therefore remains important.’
Recommended article

News • Devil in the details
Why healthcare researchers must be wary of misusing AI
An international team of researchers advises that strong care needs to be taken not to misuse or overuse machine learning (ML) in healthcare research, despite all of its benefits.
Radiologists need to optimize their current scanners to obtain the lowest possible dose levels for sufficient image quality. ‘Only if you optimize scan protocols properly on a regular scanner either for optimum resolution or low dose, then a fair comparison can be made with a new scanner with respect to dose and resolution.’
As scan protocols and scanner options become increasingly complex, workflow optimization tools gain importance. Even simple tools, for example a camera to automatically place the patient at the centre and extract body contours, will help further reduce dose. ‘Automation is quickly becoming a new frontier in CT development to increase throughput, reduce errors and limit examination costs,’ he concluded.
Profiles:
Cynthia H. McCollough is Professor of Medical Physics and Biomedical Engineering Director of the CT Clinical Innovation Center and X-ray Imaging Core at Mayo Clinic in Rochester, Minnesota, US.
Mathias Prokop is Professor of Radiology at Radboud University Nijmegen and Chairman of the Department of Medical Imaging at Radboud University Medical Center and Chairman of Radiology at the University Medical Center Groningen, the Netherlands.
06.10.2022