Article • Imaging modality comparison presented at RSNA 2024
Photon-counting CT advances identification of pancreatic cystic lesions
Pancreatic cystic lesions – indicating an increased risk of pancreatic cancer – are an occasional incidental finding in routine computed tomography (CT) abdominal imaging. New research suggests that the superior image quality of photon-counting CT (PCCT) can help detect more of these lesions. At the RSNA annual meeting, an expert outlined the benefits and limitations of the imaging technique for early detection.
Report: Cynthia E. Keen

Patients with pancreatic cysts may be at increased risk for pancreatic cancer. Therefore, an MRI scan with intravenous contrast for follow-up of incidental cystic lesions is usually performed, and guidelines recommend follow-up CT imaging on an ongoing basis. The lesions are only identified as incidental findings in fewer than 3% of routine abdominal CT scans performed, compared to up to 44.7% in MRI examinations. Recent research at multiple academic centres explores the effect of improved CT image quality on detection rates for pancreatic cystic lesions.1
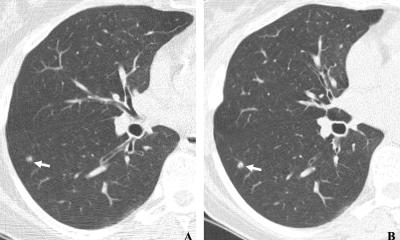
Researchers at the University of Freiburg evaluated the image quality and diagnostic accuracy of PCCT compared to conventional energy-integrating detector CT (EID-CT), with MRI serving as the reference standard. They reported at a RSNA 2024 scientific session that PCCT does improve detection and delineation, particularly for smaller cystic lesions. Additional benefits included significantly lower radiation exposure while producing higher image quality and generating higher diagnostic confidence by readers.2
Improved differentiation
Principal investigator Stephan Rau, MD, and colleagues’ database included 106 consecutive patients with a median age of 62.7 years, who had a portal venous abdominal PCCT, an EID-CT, and a multi-parametric abdominal MRI performed within a six-month period. A total of 46 simple cystic lesions were confirmed on MRI: 14 greater than 10 mm, and 27 between 5 mm to 9.99 mm in size. The researchers assessed diagnostic accuracy, and qualitative and quantitative image accuracy.
Dr Rau reported image quality, lesion conspicuity, and diagnostic confidence were rated superior for PCCT vs. EID-CT on 5-point Likert scales by three independent radiologists in a blinded reading. Sensitivity for the detection of cystic lesions was significantly higher for PCCT for all lesion categories: 76.8% vs 59.4% overall, 86.4% vs 71.6% for lesions 5 mm to 9.99 mm in size, and 90.5% vs. 83.3% for lesions equal to or greater than 10 mm.
Photon-counting CT also provided better material decomposition, resulting in higher cystic parenchyma contrast. ‘From my point of view, this is the most interesting finding of the study,’ Dr Rau commented. ‘It shows that PCCT provides better evaluation of cysts components, in this case, water-like fluids. Thereby, a new possibility for future studies on differentiation of cystic lesions based on their attenuation/material decomposition could be feasible and should be evaluated.’
MRI remains the reference standard, particularly due to its superior contrast resolution and ability to characterise cystic lesions in greater detail, such as distinguishing malignant from benign features
Stephan Rau
‘The University of Freiburg has already integrated PCCT technology for clinical applications, including abdominal imaging,’ Dr Rau told European Hospital. ‘The results of the study underline its value in improving diagnostic workflows for detecting pancreatic cystic lesions, especially in routine scenarios or where MRI access is restricted. Adoption for broader use in the specific context of pancreatic cystic lesions detection will likely depend on further advancements, including multispectral imaging capabilities for lesion characterisation.’
Asked about the potential of PCCT as an appropriate substitute for MRI, Dr Rau advised, ’MRI remains the reference standard, particularly due to its superior contrast resolution and ability to characterise cystic lesions in greater detail, such as distinguishing malignant from benign features. MRI’s unmatched soft tissue contrast, especially on T2-weighted sequences and diffusion weighted imaging, is critical for comprehensive pancreatic cystic lesion evaluation.’
He added, ‘MRI remains indispensable for follow-up imaging or cases with non-conclusive CT findings. And it does not use ionizing radiation.’ Dr Rau believes that PCCT, with its higher image quality and lower radiation dose, demonstrates great promise as a complimentary tool to MRI. ‘It may even be a substitute on scenarios where MRI availability is limited, or patients are contraindicated for MRI,’ he said.
Diagnostic boon, but a burden on workload
But while PCCT’s higher sensitivity for detecting small pancreatic lesions is a significant advantage, this technology has brought a new challenge: what should radiologists do about these increasingly common incidental findings?
Dr Rau explains that current guidelines, based on conventional CT technology, recommend follow-up imaging for all pancreatic cystic lesions. ‘This approach may impose a substantial burden on healthcare systems without clear evidence of benefit. Balancing early detection with the cost and practicality of follow up care is an important consideration for future research and policy discussions.’
Profile:
Stephan Rau, MD, is a radiologist specializing in computed tomography at the Clinic for Diagnostic and Interventional Radiology at the University of Freiburg, Germany. He has conducted extensive research in the diagnostic capabilities of photon-counting detector CT technology. His clinical research includes PCCT imaging of cystic renal lesions, the spine, head and neck scans in patients with dental hardware, multiple myeloma, and of patients with metal artefacts.
References:
- Dane B, Kim J, Qian K, et al.: Pancreatic cystic prevalence and detection with photon counting CT versus conventional energy integrating detector CT. European Journal of Radiololgy 2024;175:111437.doi: 10.1016/j.ejrad.2024.111437
- Rau S, Stein T, Rau A, et al. Detection of cystic lesions of the pancreas: Imge quality and diagnostic accuracy of photon-counting detector conventional energy-integrating detector CT |T1-SSG09-01. 2024 RSNA Meeting Central. Accessed online 26 January 2025.
26.02.2025