Image source: Adobe Stock/Monster Ztudio
Article • Knowledge gaps in gender medicine
Covid-19 and sex: higher mortality of male patients
The Covid-19 pandemic has affected scientific research in numerous ways – for example by highlighting knowledge gaps in gender medicine. In many studies differences in morbidity and mortality between women and men surfaced incidentally. While the extent and causes of these differences remain largely unexplored, the preliminary insights confirm the need for further research.
Report: Dr Christina Czeschik
As early as spring 2020, studies of Covid-19 patients in China indicated that mortality among men was higher than among women. Data from Italy corroborated these findings and at the same time suggested that more women than men were infected.1 The latter result however was not confirmed consistently: other studies reported either identical infection rates among men and women or even higher rates among men.2 Quickly, a causal relationship was established between the expression of the ACE2 receptor, which works differently in men and women.3 ACE2 is an enzyme whose membrane-bound form is Sars-CoV-2’s entry point to cells.
In many tissues of the female body, ACE2 expression is higher than in tissues in the male body, among others due to the fact that the ACE2 gene is located on the X chromosome. The genes on the second X chromosome of women are largely “silenced”, i.e. they are not expressed in the quantity, as one would assume, but are inactivated. This silencing however is incomplete: in the presence of two X chromosomes ACE2 is expressed 110% compared to the expression rate when only one X chromosome is present.4
This might explain the higher incidence of Covid-19 in women: women, the assumption goes, have more entry points for SARS-CoV-2 on their cell membranes.1
But how can the lower mortality of women be explained? Lower mortality in women remains statistically significant even when the data is adjusted for other factors such as age, life style, previous diseases, time of onset of therapy, etc. The same holds true for the fact that men are at a higher risk to develop a severe Covid-19 infection. The stats: a meta-analysis of 90 studies has shown that men compared to women have a so-called odds‘ ratio (OR) of 2.84 for ICU admission due to Covid-19 and an OR of 1.39 for Covid-19-caused death.
One possible explanation is the fact that the genes of certain proteins that the immune system needs are located on the X chromosome and thus are slightly overexpressed in women compared to men. An example would be TLR7, which plays an important role in fighting viral infections.
The male immune system and the cytokine storm
In a system that is as complex as the human immune system it would be misleading in a given situation to talk about a “stronger” or “weaker” defence against a certain virus and consider the first one to be tied to a more favourable prognosis. Indeed, certain functional impairments or organ damages are caused by the activities of the immune systems rather than by the virus itself. Following a Covid-19 – or other – infection, men are more likely to develop a so-called cytokine storm, i.e. an excessive response to an inflammation which is caused among others by the cytokine IL-6, a protein that is expressed in men to a higher degree than in women. The damage caused by the cytokine response, which often leads to severe acute respiratory syndrome (Sars), explains for example the efficacy of glucocorticoids, which in fact are an immunosuppressant, in severe Covid-19 cases. Moreover, there are indications that reduced testosterone levels in male patients might improve their Covid-19 prognosis.5
The beneficial effect of oestrogen on Covid-19 mortality was shown in a Swedish study which included postmenopausal women.6 Patients who received an oestrogen replacement had lower Covid-19 mortality rates than patients without such hormone substitutes. Whether the opposite is also true, i.e. patients with an anti-oestrogen therapy after a breast cancer diagnosis have a higher Covid-19 mortality due to the lower oestrogen levels, has not been established conclusively.
Again, the interaction is complex: some researchers assume that the less severe Covid-19 course in women can be attributed among others to the lower (rather than higher) expression of ACE2 particularly in the lung tissue of women.7
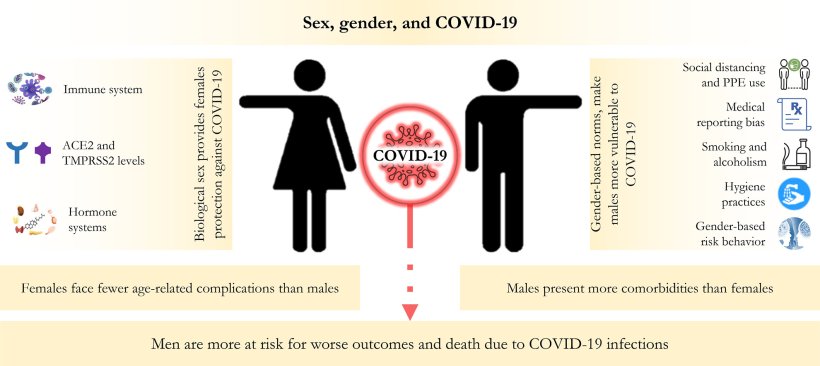
Image source: Mourosi et al., Infection, Genetics and Evolution 2022 (CC BY 4.0)
Gender medicine: relevant for all, no matter which sex
This brief look into the research on Covid-19 and sex shows that the relationships and interactions between sex hormones, immune system and specific viruses are complex. A better understanding of these factors could improve therapies for given diseases for both sexes as it might pave the way for new approaches or confirm efficacy of known medicines.
Some researchers point out that the role of sex was insufficiently taken into consideration during the pandemic.8 A review found that only about 18% of the clinical studies published during the first year of the pandemic contained gender-specific sub-group analyses. A recent survey9 conducted with the participation of the Institute for Social Medicine at the Charité and the German Medical Women's Association (Deutscher Ärztinnenbund) found that only nine of the 16 interviewed virologists were aware of the fact that there are sex differences in Covid-19 epidemiology; only three considered sex-specific differences in their discipline, virology, to be important. New approaches are required if infectiology and immunology are to progress towards truly individualised medicine.
Literature:
- Gagliardi et al.: ACE2 expression and sex disparity in COVID-19; Cell Death Discovery 2020
- Peckham et al.: Male sex identified by global COVID-19 meta-analysis as a risk factor for death and ITU admission; Nature Communications 2020
- Ortolan et al.: Does gender influence clinical expression and disease outcomes in COVID-19? A systematic review and meta-analysis; International Journal of Infectious Diseases 2020
- Tukiainen et al.: Landscape of X chromosome inactivation across human tissues; Nature 2017
- Chislett et al.: 5-alpha reductase inhibitors use in prostatic disease and beyond; Translational Andrology and Urology 2023
- Sund et al.: Association between pharmaceutical modulation of oestrogen in postmenopausal women in Sweden and death due to COVID-19: a cohort study; BMJ Open 2022
- Mourosi et al.: The sex and gender dimensions of COVID-19: A narrative review of the potential underlying factors; Infection, Genetics and Evolution 2022
- Brady et al.: Lack of consideration of sex and gender in COVID-19 clinical studies; Nature Communications 2021
- Schluchter et al.: Virologists' Sex- and Gender-Based Medical Knowledge of COVID-19 Affects Quality of Students' Education; Women's Health Reports 2023
04.12.2023











