Child diabetes cases set to soar across Europe
Mark Nicholls reports
Expert advises specific strategies should be developed to deal with this relatively new patient group.

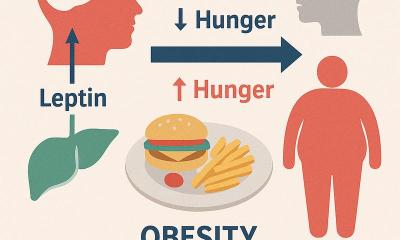
New research forecasts that child diabetes cases across Europe are set to rise significantly. Although lifestyle changes, obesity and lack of exercise are among concerning factors, it is acknowledged that more research is still needed to identify the key causes of the increase.
The majority of cases in children are type 1 but there is now a growing number of type 2, or late-onset, diabetes traditionally seen in adults.
Research, as part of the EURODIAB (Epidemiology, aetiology and public health aspects of diabetes mellitus) Study Group – a collaboration supported by the EU’s Framework Programmes – has highlighted how the number of under-five-year-olds in Europe with type 1 diabetes is set to double between 2005 and 2020 and warns that cases in older children will also rise substantially.
The study is based on 29,311 cases of type 1 diabetes recorded in 20 European centres between 1989 and 2003. The researchers, from Queen’s University, Belfast, and Pecs University, Hungary, found the overall incidence of type 1 diabetes rose by 3.9% per year. However, among the under-fives it was 5.4% a year and in the 5-9 age group, 4.3%. They calculated that, on present trends, 24,400 new cases will be diagnosed in children under 15 in 2020, including 7,142 cases in the under-fives. Prevalence in children under 15 is set to rise from 94,000 in 2005 to 160,000 in 2020.
The researchers said that hospitals will see more patients with severe diabetes complications presenting at a younger age and warned: ‘In the absence of any effective means to prevent type 1 diabetes, European countries need to ensure appropriate planning of services and that resources are in place to provide high-quality care for the increased numbers of children who will be diagnosed with diabetes in future years.’
Meanwhile, in the UK, experts believe that children with type 2 diabetes are not receiving the help they need. Dr Julian Hamilton-Shield, consultant paediatrician at the Bristol Royal Hospital for Children, led a study of 73 adolescents with type 2 diabetes and found that they put on more weight over a year, rather than losing it.
The prevalence of type 2 diabetes in adolescents in the UK and Europe is still low compared to the USA, but he fears this may not continue. ‘Addressing the obesity epidemic in childhood may halt the process, but how to do this effectively remains to be discovered.’
There are a number of initiatives across Europe aimed at reducing childhood obesity by increasing physical activity and changing diet and nutrition, such as the UK’s Change4Life campaign and Dr Hamilton-Shield’s centre in Bristol has an award-winning clinic that has had success in combating childhood obesity. However, he advocates radical help from the NHS in the more severe cases if children with type 2 diabetes are to lose substantial amounts of weight and have any chance of a normal, healthy life.
One option is a bariatric band placed around the stomach to restrict the amount a child eats. This is controversial and only conducted in a small number of cases but, while he acknowledges there are no randomized control trial studies, small cohort studies indicate that 90% of patients lost so much weight they were no longer diabetic after a year. He also believes there is sound economic reasoning for the treatment. ‘The case for surgery would be quite strong. You have to look at the total cost of drug therapy for someone with type 2 diabetes at aged 15. They will probably have it for 30 years – as I don’t think they are going to live to their 60s.’
Researchers also highlighted how most UK paediatric diabetes clinics are geared towards the treatment of type 1 diabetes, with little focus on type 2.
Dr Hamilton-Shield’s study concluded: ‘Given the rising tide of type 2 diabetes in children, the figures indicate an urgent need to develop specific strategies to deal with this relatively new patient group, with culturally sensitive lifestyle and behaviour changes as the cornerstone of therapy.’
17.09.2009