Breast screening in the Netherlands
The Dutch screening programme, which began in 1990, invites women aged 50-75 years for mammography screening every two years. Today, the national programme is undergoing considerable regional re-organisation. As one of a team of 12 radiologists at the Alkmaar Medical Centre, Dr Shirley Go is responsible for Mammography and Screening in a large Dutch region. Daniela Zimmermann, asked Dr Go about the changes in the programme's structure and the use of ultrasound, mammography and tomosynthesis in her work.

‘Our screening organisations have had to amalgamate for economic reasons,’ Shirley Go explained. ‘Up to now about 98% of the screening is still analogue, but for radiologists things are changing. Due to digitisation of mammography, the organisations want fewer screening locations.’ Screening was covered by nine different regions, but, for economic reasons, the organisations have to merge. The Alkmaar and Amsterdam regions merged this January, with Utrecht which is now a large region, with headquarters to be based in Amsterdam.
Screening is completely outsourced in the Netherlands, she pointed out. It is not carried out in hospitals, but in mobile units, or in a few non-mobile units that are also outside the hospitals. Since 1990, the LRCB in Nijmegen has organised training sessions for radiologists and radiographers and it provides certification on completion, which allows them to screen women. ‘You also have to screen a minimum of mammographies each year,’ she added. The LRCB wants to organise refresher training, in which all screening radiologists are trained to use the BIRADS -classification in screening. In the last few years, we have organised our own half-day training, for all our region’s radiologists (about 40), which involved cases and a focus on the BIRADS classification.
‘The strength of the Dutch screening programme lies in its now massive coverage. The mobile screening units drive into even the smallest villages, and invite all the women in that area to come to where the unit is stationed. After screening, all the mammograms are presented after a few days to the radiologist in that particular region, who looks at them and gives it a plus or minus, she explained. ‘The positive ones go directly to one of the many hospitals in our region. And because all the screening radiologists are everywhere in the hospitals, the knowledge and experience are established.
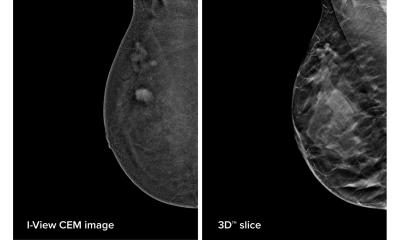
Currently most women who come to the Alkmaar Medical Centre are symptomatic (have a breast complaint) and have a mammography and if necessary an additional ultrasound. However, last September, this was the first hospital, worldwide, to put into clinical practice a commercial tomosynthesis machine manufactured by Hologic. This is another tool to examine women in the search for breast cancer, but in our clinical setting we can also rely on what we can feel with a physical examination and what we can see using ultrasound. So, I think tomosynthesis is a nice machine, because it gives you more about the architecture and the structure of the breast, but because we’ve only had this machine for a few months, if I see something, I don’t say, “Okay, I have my tomosynthesis images, I am not worried anymore, I will not perform an ultrasound”. But I’m used to doing an ultrasound.
‘There is one important thing to know: all machines have many problems when they are new. We have technical problems with post processing and so on, but now the machine is working properly. We’re happy to have it in our hospital, with its large region to cover and a large number of breast care patients.’
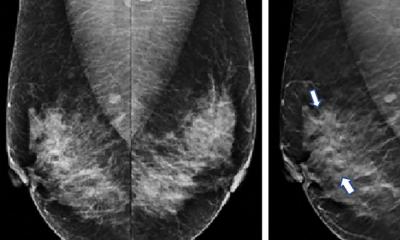
So, will using tomosynthesis make the work quicker? ‘Well, the US has got all the scientific numbers and results from its screening programmes, but it is differently organised there than in Holland, Scandinavia, or Germany. And, because the US referral percentage is much higher, they are more careful because of lawsuits and so on. In Holland our referral number is about one fifth of the number of the women referred in the US. There, for example, after screening, hundreds of women are sent for assessment, whereas in Holland we send about 20 for referral after a positive mammogram.’ A mammogram, she explained, ‘is a two-dimensional image, so everything inside the breast is imaged on top of each other. An image on the tomosynthesis projects the tissue, as if you can scroll through the tissue. So, for example, if I thought, “Well, is there a lesion, is there some abnormality?” then with tomosynthesis I can scroll through the breast and see, “Oh, it’s just breast tissue, it is okay.” But combining a mammogram with tomosynthesis makes it easier and makes us more confident in our diagnosis.’
So, in future, the referral rate will go down if using tomosynthesis and money will be saved? ‘Maybe -- I don’t know. We will decrease the number of referrals using tomosynthesis in the Dutch screening programme since our number is already that low, especially compared with the US. However, this will not happen, because we are not going to use tomosynthesis in the Dutch screening programme, but regular digital mammography. Perhaps in the future but for now we only use tomosynthesis in the hospital. We made a list of which women we would send primarily for tomosynthesis. For example women referred from the screening programme: they will have tomosynthesis and mammography, both examinations in one procedure. And so will high risk women who have a family history of breast cancer, in whom we know they have dense breast tissue or when they come for the first time.
If I can choose between tomosynthesis or ultrasound additional to X-ray, I’d choose ultrasound if I saw some abnormality on the mammogram, or if there was a lump somewhere. I would not do an extra tomosynthesis image. Not yet.
‘We only use MR for those at very high risk; for example, women with genetic defects. The women who have a slightly raised risk because of a family history of breast cancer, but not with a genetic defect, we screen them as well, but with mammography and, if we have tomosynthesis, with that. In Holland up till now there are only a few machines that can do tomosynthesis, because it is so new most of the hospitals don’t have it. It is also expensive, because you also need a dedicated monitor and post processing stations to review, because you can’t look at the images on our normal screen.’
The radiographers are very pleased with the new tomosynthesis machine, Dr Go added, ‘because it’s very easy using the touchscreen. Another advantage is the tungsten filter; the radiation dose is less than from the older mammography machine. The only thing is that, we’ve had some technical problems at the beginning, which Hologic is solving at the moment. So, it’s all in the game, but we are quite happy with all our equipment. It makes my work very easy and comfortable.
‘For me, I don’t yet know if tomosynthesis will help as much as expected from the numbers of the scientific reports from the States. They talk about 40% fewer biopsies, less referrals. As I said, we work differently here, so I don’t think it will help me for that side, but what’s most important is that I have the choice of which modality is best for a particular woman.
‘In the future, perhaps tomosynthesis will reduce our number of ultrasounds, especially if you look, for example, at a mammogram and think it may be tissue or not, or there is something there, and then I have the tomosynthesis images and don’t worry anymore; it’s clear. I think it will help us in the future, but it is still very fresh.’
07.03.2009