Breast cancer early detection – quo vadis?
Risk assessment and new technologies shape the developments
Why is early detection of breast cancer so important? Professor Dr Walter Heindel, Director of the Institute of Clinical Radiology at University Hospital Münster, Germany, offers an unequivocal answer.

“Breast cancer is the most frequent tumor disease in women and at the same time the most frequent tumor-related cause of death in women”. In view of these facts Germany – just like many other countries – introduced a screening programme several years ago with the aim to detect breast cancer in its pre-clinical phase, i.e. before symptoms appear. According to the Robert Koch Institute, in Germany 75,000 new diseases are recorded each year and more than 17,000 women die due to the aggressiveness of some tumor types and the development of metastases. Thus early detection is crucial – for every single woman and for public health policy at large, the Dr Heindel emphasizes.
Major aim: objectifying screening results
The statistical aim of early detection is decreasing mortality. While screening programmes offer every woman the possibility to have minute tumors detected, epidemiologically speaking the effects of decreasing mortality, as of today, can only be assessed in seven to ten years. A study to analyze the epidemiological effects of mammography screening, commissioned by the German Federal Ministry for the Environment and the German Federal Ministry of Health and supervised by the Federal Office for Radiation Protection, was recently launched at the University of Münster. The German state of North-Rhine Westphalia was chosen because the most populous federal state maintains a well organized cancer registry – a precondition for meaningful statistical results. “Objectifying the screening results is important to determine the benefits and risks of screening and to show that the highly publicized drawbacks such as radiation exposure and false-positive findings that lead to stress for the women concerned and require extras biopsy resources are outweighed by the benefits of the screening procedure,“ Professor Heindel explains.
X-ray-based mammography: method of choice for women with normal risk
Today, screening is usually performed with digital mammography (DM). This technology yields good results in women between the age of 50 and 69 with normal, meaning less dense breast tissue as it detects lesions from approx. 5 mm. Very dense tissue, rather rare in this age group, may impede the detection of small masses.
DM technology is being developed along different routes such as the so-called photon counting or innovative flat panel detectors all with the aim to provide high resolution digital mammograms at very low dose. Exposure reduction is currently a major research objective worldwide particularly with the radiation-sensitive breast tissue in mind.
MRI for high-risk women
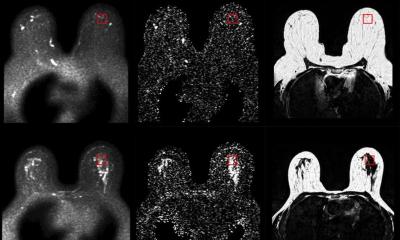
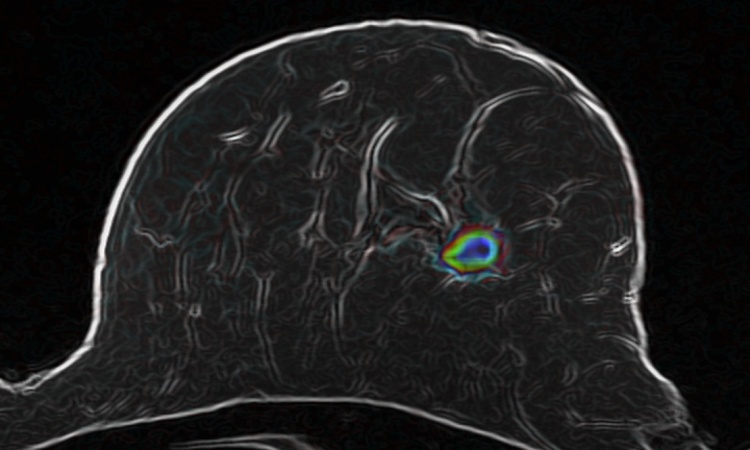
The normal, sporadic life-time risk for women to develop breast cancer is ten percent. For this group x-ray-based procedures are the method of choice. While high risk is defined to begin with a 30 percent probability to develop the disease there is the very high risk (80 percent) group of women who carry the BRCA gene. These women, who frequently have cancer at an early age and also frequently develop cervix carcinoma, are screened in 15 centres in Germany using MR mammography. A few years ago the so-called EVA study, supported by Deutsche Krebshilfe (German Cancer Aid), gained worldwide acclaim for its valuable information on the use of different imaging modalities to detect breast cancer in high-risk women. More than 90 percent of all lesions larger than approx. 5 mm are detected with contrast-enhanced MRI. The tumors in these young women are often particularly aggressive and do not respond to hormone therapy which makes them very difficult to treat.
A further group is defined as having a risk between 15 and 30 percent where breast cancer is associated with other genes that are clinically not as dominant as BRCA, family risk and risk lesions.
Setting the course for better outcomes
“Firstly, diagnostics has to be tailored more precisely to the three risk groups and their particular needs. Every woman should determine her personal risk with her physician,” Professor Heindel recommends.
Secondly, there are new technological options such as tomosynthesis where a radiation source rotates around the breast to acquire slice images which then are used to create 3D images similar to CT scans. To analyse calcifications and to be able to compare these images to previously acquired scans, 2D images can be reconstructed. The angle at which the radiation source is guided around the breast during tomosynthesis is still being discussed; exposure with this technology is comparable to 2D mammography. Current studies from Norway and Italy indicate increased tumor detection rates of up to 30 percent. “I expect this technology to prevail”, Heindel says and proposes a randomized multi-center study on this diagnostically intricate and expensive method to convince the decision makers in healthcare politics.
MRI is moving from 1.5 Tesla to 3 Tesla with even higher resolution. One advantage of this improved field strength might be the detection of ductal carcinoma in situ (DICS), a pre-cancer form. Non-contrast diffusion weighted MRI which measures the altered mobility of molecules in tumors also promises enhanced diagnostic capabilities.
MRI is not the only modality to present technological innovation: while elastography in ultrasound is not yet sufficiently evaluated for breast cancer early detection this method might nevertheless support diagnosis in dense tissue and thus is, as Professor Heindel points out, “another valuable research subject”.
Profile:
Professor Dr Walter Heindel is Director of the Institute of Clinical Radiology and Director of the Reference Center “Mammography” at the University Hospital Münster, Germany. His research focuses on the role of imaging in early detection (such as breast cancer screening) and innovative minimally invasive, image-guided treatment options.
04.12.2013