Article • Breast cancer screening
Benefits must outweigh risks
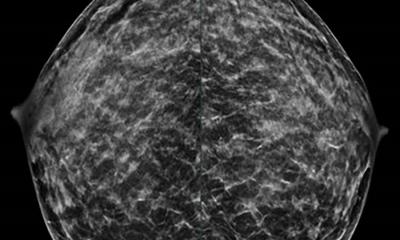
Biannual mammography can help to reduce breast cancer mortality by 40% in women aged 50-69, but the benefits for women under 35 years old are questionable, eminent Spanish radiologists highlighted during a session held by SERAM, their national society of radiology, last November, during the International Radiology Day.
Report: Mélisande Rouger
‘Mammography today is the only method that has demonstrated capacity to reduce breast cancer mortality. Only in high-risk patients is MRI a proven screening method,’ said Dr Marina Álvarez Benito, President of the Spanish Breast Diagnostic Imaging Society and a radiologist at the Reina Sofía Hospital in Córdoba.
Biannual screening reduces mortality by 40%

A study recently published in European Radiology showed that early detection through biannual mammography in a screening program reduces mortality by 40% in women aged 50-69. But there is less evidence for women aged 40-49 and over 70. ‘Actually, for women between 35 and 40 there is very little evidence regarding associated risk factors or patient specific situations,’ explained conference speaker Dr Carmen Carreira, a radiologist at Fuenlabrada University Hospital, in Madrid, and a member of the executive committee of SEDIM.
Cancer incidence is very low in a breast cancer screening program – on average five per thousand, Álvarez estimates. This means it is crucial to weight the benefits of screening against the potential risks, she added.
Benefits must outweigh potential risks
‘The women who take part in a screening program are healthy and most of them will not develop cancer; it’s very important to remember that benefits must outweigh potential risks.’ Both radiologists’ comments came a month after the Spanish Society of Gynaecology and Obstetrics issued recommendations advising women to undergo their first clinical exploration together with a mammography as early as 35 years of age, to determine their breast type and morphology, an indication on their potential predisposition to develop cancer (http://www.efesalud.com/noticias/primera-mamografia-los-35-anos/).
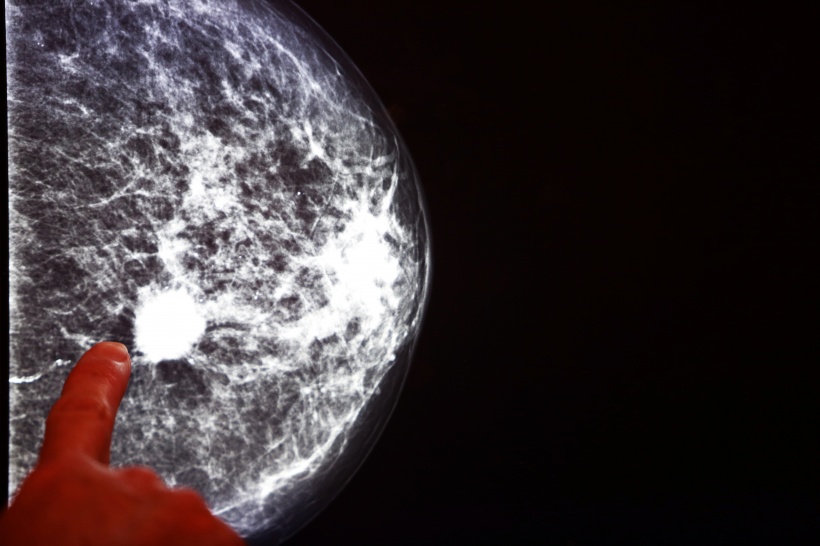
The SERAM asked all parties involved to avoid sending confused messages on breast cancer screening program, which was initiated in the early 1990s in Spain; instead, women should be informed in a clear and transparent manner. ‘The chance of saving a life thanks to early breast cancer detection is 100% superior to the possibility of death caused by the radiation used in the examination,’ the society wrote in a release.
Benefits of mammography include mortality reduction and the possibility of conservative treatment. Most common potential risks would be false positives, over diagnosis, overtreatment and the detection of harmless lesions that will trigger useless biopsies and anxiety in the patient. ‘Benefits will only affect a small part of the women whereas potential risks will affect all women who take part in a screening program,’ Álvarez pointed out.
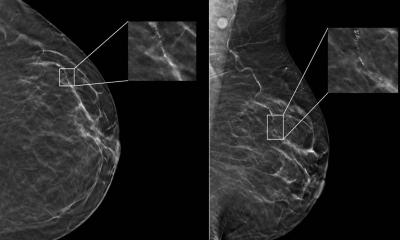
The possibility for false positives in a woman who has taken part in 10 screening programs, i.e. during 20 years of her life, is around twenty percent. The only way to improve screening efficiency is to have quality controls at every stage of the program, Álvarez believes. The European guidelines offer a wide range of indicators to evaluate false positives, including the number of recalls. ‘To have what we call a good false positive rate, recall rates should not rise over 7%. For a program to be efficient, 70% of the women should participate on a regular basis, and not just one time,’ Álvarez said.
Know the route from primary to secondary care
Adherence to the program is key and doctors must follow their patients between primary and secondary care to guarantee the proper chain of actions. ‘It’s relevant to know a woman’s circuit from the detection of a lesion in primary care to her management in secondary care,’ she said. ‘One key element here is to communicate screening results within 15 days of the examination.’
Radiologists and radiographers should also undergo dedicated training in breast imaging. Technicians must know how to position and compress the breast, and be able to assess examination quality. ‘For radiologists the learning curve is extremely long,’ she emphasised. ‘They need to dedicate a very significant amount of their time to training and practice.’
Profile:
Marina Alvarez Benito is Director of the Clinical Management Unit of Radiology and Breast Cancer at Reina Sofía University Hospital in Córdoba, Spain. She is also the current President of the Spanish Society of Diagnostic Breast Imaging. The expert received a bachelor degree and doctorate in medicine and surgery from Córdoba University. A former member of the Board of SERAM, she currently works in partnership with the Society.
04.08.2017