Photo: Juliette van Haren / Industrial Design
News • Incubator 2.0
Artificial uterus improves odds for preemies
“An artificial uterus – the incubator 2.0 – will become a reality within 10 years,” says Jasmijn Kok, one of the founders of Juno, a spin-off from the Eindhoven University of Technology, Netherlands.
Together with researchers from the department of Industrial Design from the University, including her twin sister Lyla Kok, she wants to bring a technology that increases the chances of survival of extremely premature babies to the market. “It’s not science fiction.” What once started as a wild idea, a moon shot, is now taking shape, co-founder Myrthe van der Ven continues. At congresses in Japan in the 1970s, gynecologist Guid Oei first saw initial ideas for accommodating extremely premature babies not in an incubator, but underwater in an artificial uterus.
The important thing is that parents accept the technology and that care providers enjoy using this device. They shouldn’t see it as something technical, but something that is necessary for the child to survive
Myrthe van der Ven
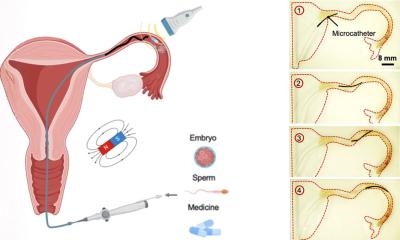
In extremely premature infants, the organs are not yet fully developed. The lungs in particular need fluid from the uterus. In the current incubator, they receive breathing support and keep their hearts are kept beating, Van der Ven points out. “Actually, a premature baby – a neonate – is not yet ready for that support. There’s a high risk it will die. In the long term, infants may continue to have problems with breathing or with the circulation of oxygen to the brain. We expect them to continue to develop in a simulated womb as they would in the natural womb.”
The spin-off – named after the Greek goddess of life and birth, Juno – stems from a European consortium. It received €2.9 million in European grants in 2019 to develop an artificial uterus.
In addition to the necessary hardware, there is a software side. In the new incubator, sensors monitor how the premature baby develops. The researchers are also using digital twin technology. Mathematical models, measured and available data, and artificial intelligence mimic the neonate. This allows the researchers to advise and assist physicians with choices in neonatal care. “We are still looking for a name for a premature baby in an artificial uterus,” says van der Ven.
The tests are done with 3D-printed practice mannequins. These come in all sizes and weights. Coupled to a digital twin model, a real baby’s response to treatment can be simulated, explains de Van der Ven. “That all still sounds very technical. The important thing is that parents accept the technology and that care providers enjoy using this device. They shouldn’t see it as something technical, but something that is necessary for the child to survive. We have to take that step toward acceptance as well.”
One of the biggest challenges is that the fetus, aged 24 to 28 weeks, does not gasp for breath just after birth. American professor Alan Flake has already shown that it is possible to anesthetize a lamb and allow it to continue developing underwater in an artificial uterus. “We want to make the transition to the artificial uterus as natural as possible,” says Kok. So the research focuses not only on the artificial uterus itself and how the premature baby is fed through the umbilical cord by an artificial placenta but also on how the delivery should proceed.
Recommended article
News • Neonatology
Artificial womb supports lamb fetus, may save extreme human preemies
A unique womb-like environment designed by pediatric researchers could transform care for extremely premature babies, by mimicking the prenatal fluid-filled environment to give the tiniest newborns a precious few weeks to develop their lungs and other organs.
There are still ethical dilemmas to overcome, says van der Ven. “We will certainly pay attention to that. For example: How are we going to prepare society for this new technology? What is allowed and what is possible? What children would be the first candidates for this? We have to answer questions like that, of course.” In the Netherlands, for example, you are not allowed to save a neonate younger than 24 weeks, Kok continues. “That’s laid down here. In Scandinavia and Germany, that limit is set at younger than 23 weeks.” The researchers also need to look at other countries. “The Netherlands, with about 600 babies a year that we could help, is actually too small a market for such a complicated medical product. We need to investigate what other cultures think and what their legislation is.”
Ultimately, it would be great if this technology could also be used in developing countries, says van der Ven. There, the death rate of newborn babies remains alarmingly high, according to a study by Unicef. “In the early stages it’s still very pricey, but we’re definitely keeping that in mind.” Kok: “We first need to prove that the technology works and the concept is right. Then we can continue to develop to make it simpler and cheaper.”
The spin-off is part of a larger partnership conducting research into a “Perinatal Life Support” system. Partners include the universities in Eindhoven, Netherlands; Aachen, Germany; and Milan, Italy; plus the companies LifeTec Group, Nemo Healthcare, MSB de Medici and Medsim. In 2024, the funding from Horizon 2020 will end, by which time the prototype of the artificial uterus should be ready. After that, the preclinical and clinical tests and the certification process will start.
Source: Eindhoven University of Technology
09.10.2021