Cancer diagnostics I
Ambiguity calls for a second opinion
Each year, approximately 1.6 million women in the USA have breast biopsies to diagnose or rule out cancer. Pathological diagnosis is considered the gold standard – how accurate are these diagnoses?
Report: Cynthia E. Keen
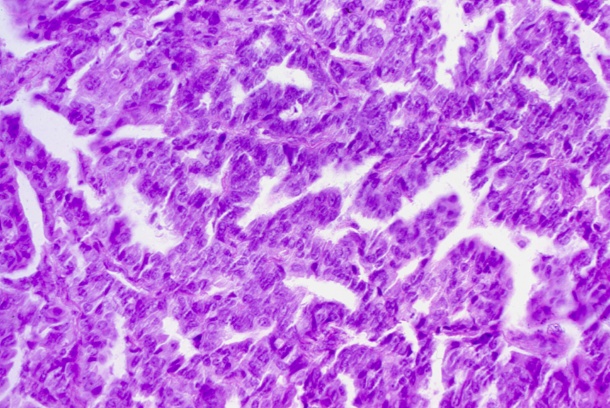
A recent study published in the Journal of the American Medical Association that generated national media headlines has shaken the faith of American women and their doctors. 115 pathologists, working throughout the country, independently interpreted biopsy samples of 60 cases. Whilst their diagnoses of invasive breast cancer were nearly 100% accurate, one in five pathologists made incorrect diagnoses relating to ductal carcinoma in situ (DCIS), and half misdiagnosed the presence of atypia – abnormal cells.
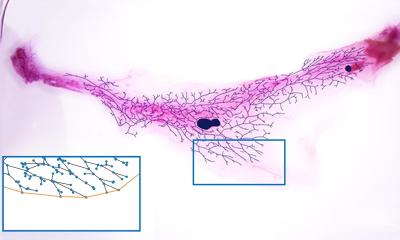
Accurate diagnosis of atypia is important. Although 87% accurately diagnosed benign tissue samples without atypia, the fact that 52% of atypia cases were misdiagnosed is disconcerting. With a diagnosis of atypical ductal hyperplasia on a core needle biopsy, further surgical excision of the site is recommended to ensure that a cancer is not missed as a result of a sampling error. Over-diagnosis of atypical ductal hyperplasia may lead to unnecessary surgery and under-diagnosis of atypia may miss a cancer in adjacent tissue.
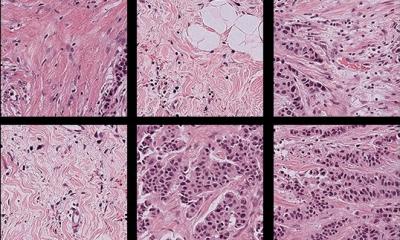
The study consisted of sending a set of 60 cases with a single tissue sample to each of the 115 pathologists. The 60 cases were a subset of 240 cases: 10% were tissue samples of invasive carcinoma, 30% DCIS, 30% atypia, and 30% benign. Diagnoses were made independently and subsequently by consensus of three expert breast pathologists.
Nearly half of the cases were from women aged 40-49, 28% from women aged 50-59, 12% aged 60-69, and 11% age 70 and over. Breast density categories from mammograms included all categories, with heterogeneously dense and extremely dense representing 40.4% and 10.4% respectively. Samples were obtained from both core needle and excisional biopsies.
Principal investigator Dr Joann G Elmore, an affiliate investigator at the Fred Hutchinson Cancer Research Center of the University of Washington in Seattle, and colleagues, reported that over-interpretation of atypia was 17% and over-interpretation of benign tissue without atypia was 13%. DCIS was diagnosed as invasive carcinoma in 3% of cases. Under-interpretation was 4% for invasive breast cancer, 13% for DCIS, and 35% for atypia.
‘We were surprised by the amount of disagreement among pathologists,’ Elmore said in a JAMA website video interview. Should she have been? The individual diagnoses of the three expert pathologists were in agreement only 75%. Only after they concurred with one another did they reach the consensus diagnoses used to compare the diagnoses of the 112 pathologists.
‘The key finding [of the study] was that the overall concordance rate of diagnostic interpretations with the reference diagnosis for participating pathologists was 75.3%, identical to the initial level of unanimous agreement between the three expert pathologists,’ wrote Professor Nancy E Davidson MD, director of the University of Pittsburgh Cancer Institute and Professor David L Rimm PhD*, director of pathology tissue services at Yale School of Medicine in New Haven, CT, in an accompanying editorial. They stated that ‘the accuracy of the pathologist’s diagnoses is relatively understudied and represents an important knowledge gap at a time when medicine is becoming more evidence-based’.
However, they pointed out factors that may have influenced the inadequate performance. Pathologists only had a single slide to work with, and did not have the option to consult with others. In daily practice, they work with multiple slides and have the ability to consult with colleagues about challenging cases. Additionally, the case mix of slides included a large number of challenging cases that were atypical of what a pathologist would encounter on a day-to-day basis.
However, because pathologists were in low-volume practices and less experienced pathologists made more errors than more experienced pathologists in the cohort, Davidson and Rim recommended that pathologists should consult with more expert colleagues about challenging cases – and, in cases of ambiguity, a second independent opinion is recommended.
*Davidson NE and Rimm DL. Expertise vs. Evidence in Assessment of Breast Biopsies. 2015 JAMA 313:11, pp. 1109-1110.
27.04.2015