Article • Cardiology & radiology
AI opens up boundaries between medical disciplines
AI-based evaluation of chest CT scans allows comprehensive assessment of different organ sections
Report: Daniela Zimmermann
Uwe Joseph Schoepf, Professor for Radiology, Cardiology and Paediatrics and Director of the Department of Cardiovascular Imaging at the Medical University of South Carolina, discusses areas of application for AI-based radiology. The cardiothoracic imaging expert and his team were largely involved in the development and early clinical trials of the Siemens AI-Rad Companion Chest CT, a software package for computed tomography (CT) based on artificial intelligence (AI).

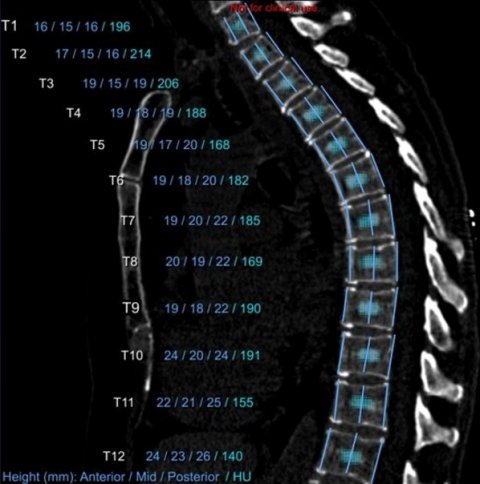
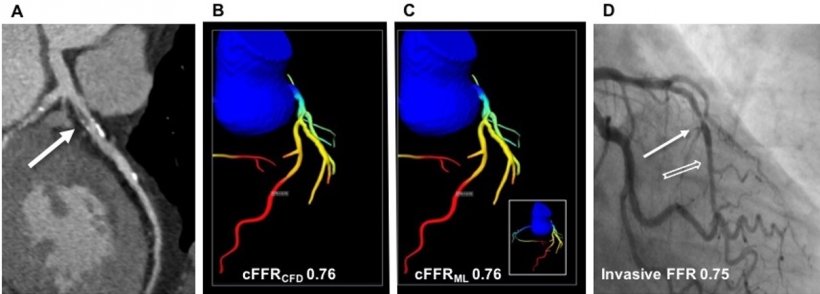
On CT scans the application can distinguish between thoracic organs, such as the heart, lungs, aorta or vertebral bodies, and detect anomalies. Achieving this ability entailed training the software with real clinical cases from Schoepf’s department, where the system was being trialled. Those trials were also used to find answers to further diagnostic questions. ‘Apart from cardiac problems, such as automatic measuring of the aorta, interdisciplinary aspects, such as how to also utilise a chest CT to determine bone density, were also of interest. Furthermore, areas of application for emphysema quantification and opportunities for the automatic detection and quantification of arteriosclerotic plaques, were also examined,’ Schoepf explains. The precision of pulmonary nodule detection achievable with this software is also currently being tested.
Focus on the patient
I believe it’s very important that patients become involved in their treatment plans and healing process
Uwe Joseph Schoepf
Schoepf believes the value of AI application lies in its versatility: ‘The applications are helpful because they deliver a comprehensive evaluation of functional imaging studies, providing us with a complete package of everything that may be important for the patient.’ This is an important step towards patient-centred medicine because the focus shifts from the individual organs to the patient, their needs and the events occurring in different organ sections.
This interdisciplinary approach requires efficient communication between the medical specialists involved. Schoepf cites an example: ‘If a radiologist is looking for plaques and then happens upon pulmonary nodules when the AI-Rad Companion Chest CT is used, they will pass on the result to the doctor in charge of treatment and may recommend further observation, a nuclear-medical examination or a biopsy.’
In the US, unlike in Germany, the patients are much more involved in their treatment. Even smaller hospitals offer increasing opportunities for all patients to have direct access to their medical records, so that they can inform themselves about results and treatment plans. Schoepf believes this trend is positive: ‘I think it’s good that patients finally can take steps to maintain their health. It empowers them and I believe it’s very important that patients become involved in their treatment plans and healing process.’
AI takes over quantifications
One large advantage of the use of AI in radiology is that it frees up valuable medical staff from laborious and time-consuming quantifications. The fear that AI will replace the radiologist has been sufficiently refuted, Schoepf underlines. ‘This won’t happen. The AI-Rad Companion is a very good example of how AI will help us to carry out work that nobody really likes doing, but which is easy for the computer.’
Some examples for this are the quantification of coronary calcium and the quantification of emphysema (which is increasingly important due to advances in emphysema treatment) along with the next, logical step – measuring the aortic root for TAVI.
Recommended article

Article • AI in imaging
Radiologists must control their own destiny
Radiologists have not ended talk about artificial intelligence and machine learning but, rather than fear for the future of their profession, they themselves must decide how that should be, an eminent expert Dr Woojin Kim warned ECR delegates in Vienna in March. Two years in discussion and the hype around artificial intelligence (AI) is far from fading. Interest has never been higher, and the…
‘The use of AI applications makes it ever easier to utilise all information contained in an X-ray or chest CT; this becomes obvious when we look at bone density measurements, which would usually require a separate, additional examination,’ the professor enthuses. All results the AI extracts from a chest image are automatically presented as a structured report so that the radiologist and referring doctor can draw conclusions for the treatment plan. This focused view into different organ areas also could be possibly used to comprehensively evaluate the effects of an individual hazard or individual cause of a disease – such as the constellation of calcified plaques, pulmonary nodules and pulmonary emphysema in smokers – in a lung cancer screening population, for instance.
The future – analyses based on deep learning
Schoepf believes that, in the future, the possible uses for AI in medicine will go way beyond the current capability of the Rad Companion. With the help of deep learning, computers could take over the independent evaluation of data sets to find correlations that, as yet, are unknown. ‘This is one of the most exciting applications per se: the computer looks at everything with “fresh eyes” and tries to find correlations for which the human brain simply does not have the neural network capacity,’ Schoepf explains.
There are already cases where a computer analyses a patient’s entire medical record. If, in future, millions of data sets become available, computers will be able to use their evaluations to make new connections, such as those between factors that cause certain diseases, impact on life expectancy or bear specific risks. Deep learning, however, makes many – and not just lay people – a little uncomfortable because the users can no longer follow the individual steps of the computer’s learning process. The expert is relaxed about this. ‘This black box principle, i.e. the fact that we don’t know why the computer makes connections, can lead to confusing results. However, ultimately, this means that we are challenged to scrutinise, examine or eliminate the results.’
Schoepf does not believe there to be a risk that AI applications could generate their own, dangerous momentum, neither under normal circumstances, nor in the distant future.
Profile:
Austrian-born Uwe Joseph (Joe) Schoepf is a professor with appointments in Radiology, Cardiovascular Medicine and Paediatrics at the Medical University of South Carolina (MUSC) in Charleston, SC. There he directs the Cardiovascular Imaging Division and is Director of Computed Tomography Research and a Director of the University Designated Centre for Biomedical Imaging. Schoepf grew up in Munich, Germany, where he graduated in medicine at Ludwig Maximilian University (LMU) and received specialist training at its Institute of Clinical Radiology. In 2001, already an accomplished radiologist, he left Munich to pursue his interest in cardiothoracic imaging at Brigham and Women’s Hospital, Harvard Medical School, in Boston, MA. The professor joined MUSC in 2004.
02.09.2019
- AI (834)
- cardiology (779)
- CT (608)
- deep learning (167)
- personalised medicine (263)
- radiology (735)
- structured reporting (13)





