What´s new in neuroradiology and interventional radiology?
When scanning seizures, Dr Walter Kucharczyk, director of MRI at Toronto General Hospital, believes that MRI still remains the best imaging test to discover if there is an anatomic or structural abnormality that might account for a seizure.
However, some centres are now combining this approach with other imaging technologies as well to improve results even further. Better imaging of lesions, combined with other diagnostic tests, has improved decisionmaking over whether surgery would be safe or not, taking into account the chances of success and risk of complications.
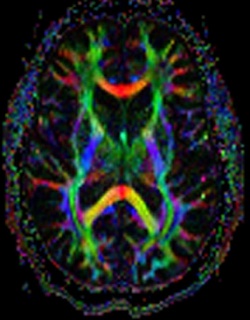
Some patients also have a PET scan, which can clarify the MRI or EEG and reduce ambiguities in test results. ‘PET is used more often for this and our finding is that PET results are fused to the MRI results,’ he said. ‘PET is very sensitive to brain biochemistry abnormalities but the image resolution is not as good as MRI, so you might get a half centimetre resolution with PET but a half a millimetre resolution with MRI.’
Many larger centres were moving towards this approach, he said, as well as using magneto-encephalography
(MEG) for brain mapping.
Globally, most MRI machines are 1.5-Tesla and are good for scanning seizures, along with the 3-T machines, but one of the current areas of discussion is over the use of 7-T to scan seizures. While the increased magnetic signal strength offers better images patients might have biological side effects. Significant improvements in image resolution from 7-T ultrahigh-field magnetic resonance (UHF MR) scanners have been achieved in recent months by replacing the multichannel radio frequency (RF) system of four coils with 16 coils.
Greater availability of MRI – and its array of applications - is high on radiologists’ wish lists due to its potential and ability to deliver excellent images without dose issues. Also progressing is diffusion MRI, which explores the micromovements of water molecules, and can produce in vivo images of biological tissues weighted with the local microstructural characteristics of water diffusion, which can show connections between brain regions.
Interventional radiology
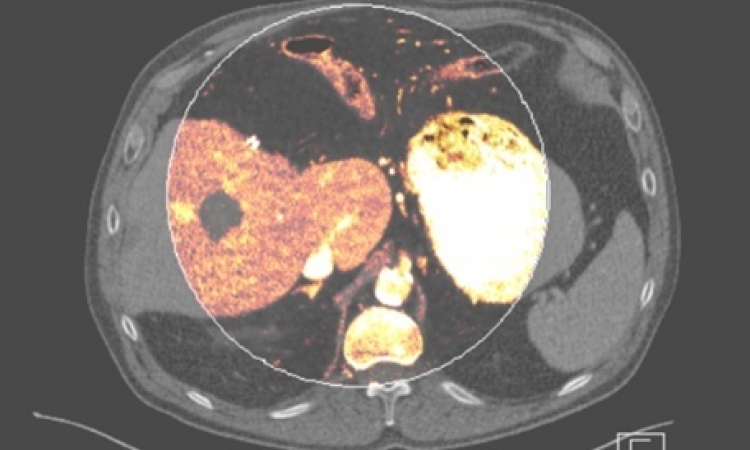
Within this, techniques demonstrating clear benefits include molecular MR imaging on a cellular and even subcellular scale; combined imaging with radiotherapy treatment delivery, e.g. MRI-Linac combinations (under development), and MRI perfusion imaging of the myocardium or MR angiography of cardiac blood flow.
An interesting development has been the evolution of training simulators, such as a computer-based virtual reality environment for training interventional neuroradiology procedures. The NeuroCath (Neuroradiology Catheterisation Simulator) system includes extraction and construction of a vascular model from different imaging modalities, to efficiently represent a patient’s anatomy.
21.02.2012