Faster scanners, more parameters, better markers…
With MRI and CT scanners widely available in clinical routine, radiologists cull increasingly precise and relevant functional tumour information for diagnostics and monitoring purposes. Both modalities offer technological and methodological approaches, initiated by the discipline itself, that have become indispensable for certain frequent tumours.
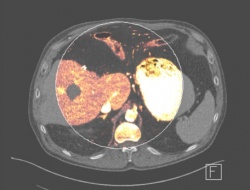
In primary diagnosis of prostate cancer for example multi- parametric MRI is a clinically established procedure today while dual-energy CT is about to become standard operating procedure for monitoring the response to gastrointestinal stromal tumour (GIST) or renal cell carcinoma therapy.
‘Multi-parametric prostate MRI usually analyses four parameters: morphology using T2-weighted imaging and cellular density using diffusion-weighted imaging; MR spectroscopy provides information on the metabolism and contrastenhanced imaging shows increased perfusion due to angiogenesis, that is new and immature tumour vessels,’ explains Professor Stefan Schönberg, Director of the Institute of Clinical Radiology and Nuclear Medicine at the University Hospital Mannheim, Germany.
The European Society of Urogenital Radiology (ESUR) has published guidelines for multiparametric prostate evaluation that include a classification system for structured reporting. Based on the individual scores of the four parameters, the final score allows the classification of the tumour according to its degree of malignancy. Dynamic contrast-enhanced imaging involves the very fast acquisition of 3-D sequences with continuous contrast media injection and the analysis of three quantitative parameters: the wash-in rate indicates average blood flow, the mean transit time is usually shorter in tumour tissue and contrast differences between the intravascular space and interstitial tissue due to weak vessel walls. While the results of contrast-enhanced MRI cannot yet exclude tumour development, Prof. Schönberg says ‘data from animal studies indicate that special volume CT scanners that offer extremely high spatial resolution can visualise angiogenesis at a very early stage. Moreover, there are targets that, in combination with substances visible in positron emission tomography, are directed towards avß3 integrines. These are structures that are typically associated with angiogenesis.’
Anti-angiogenic substances inhibit tumour growth
Neovascularisation, which in a way is the basis for tumour formation and above all tumour growth, is stimulated by the release of vessel growth-promoting substances such as vascular endothelial growth factor (VEGF). Today, attempts are made to ‘starve’ the tumour with new biological substances, such as tyrosine-kinase inhibitors, on a molecular level.
When conventional tumour therapies fail or when highly vascularised tumours are present, anti-angiogenic substances are used either by themselves or in combination therapies – an important substance being Imatinib. ‘These developments present us radiologists with new tasks. We have to monitor the efficacy of the substance over the course of the therapy with a functional diagnostic,’ the professor explains, adding that in this respect MRI has a disadvantage: used with contrast media and with high temporal resolution it can visualise only very small volumes. CT on the other hand offers two different but very interesting approaches.
‘Firstly, there is 4-D CT, dynamic volume CT with a moving table, which very much like 3-D MRI acquires sequence images with contrast media and can quantify the three perfusion parameters already mentioned,’ he explains. ‘Secondly, there is dual energy CT, which allows us to extract iodine information quantitatively as a marker for tumour perfusion – without increased radiation exposure. This approach has entered clinical routine for one tumour – GIST. We will elaborate on this approach in a multi-centre prospective study. Dual energy CT may indeed trigger a change of paradigm in general healthcare,’ Prof. Schönberg concludes.
Profile:
A medical graduate from Ruprecht-Karls- University, Heidelberg, Professor Stefan Schönberg then trained in radiology at the German Cancer Research Centre. In 2001 he joined the Institute of Clinical Radiology at Ludwig Maximilian University, Munich, initially as senior consultant and head of the MRI unit and later as managing senior consultant. Since 2007 he has directed the Institute of Clinical Radiology and Nuclear Medicine at the University Hospital, Mannheim. His research focuses on vascular and abdominal imaging, functional MRI, highfield MRI and oncological imaging.
19.11.2013





