Article • Emergency medicine
Ultrasound can save lives
‘Ultrasound plays a key role in diagnosis and monitoring of treatment in the A&E department,’ emphasises Professor Joseph Osterwalder, Medical Director of the Cantonal Hospital in Appenzell, Switzerland. ‘I cannot imagine emergency medicine without ultrasound.’
Report: Michael Krassnitzer
At the time when the DEGUM, ÖGUM and SGUM outlined the importance of ultrasound in emergency medicine in their jointly developed guidelines this caused some raised eyebrows. ‘But, we were pioneers in Europe,’ emphasises Osterwalder. ‘All the other countries are now following suit. In emergency situations, ultrasound can save lives.’

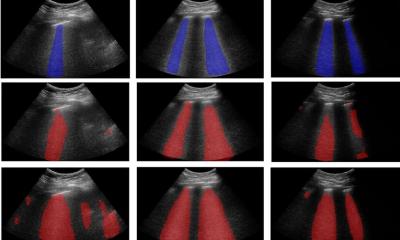
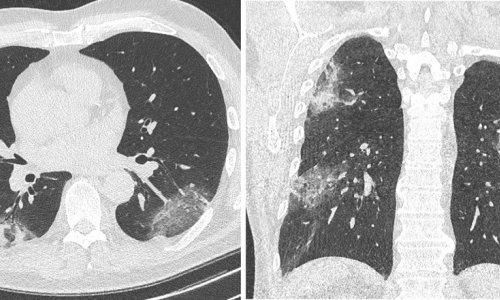
Although we can ask patients questions, carry out manual examinations, take X-rays and do full blood counts, the human body is a black box. ‘All these resources are comparatively imprecise. Ultrasound is a very valuable addition, as it provides certainty,’ Osterwalder adds. Pneumonia for instance, or an intestinal obstruction, can be detected much earlier with an ultrasound scan than with an X-ray. For a patient with severe breathing difficulties, ultrasound can even be carried out during intubation and can help diagnose a potential central pulmonary embolism.
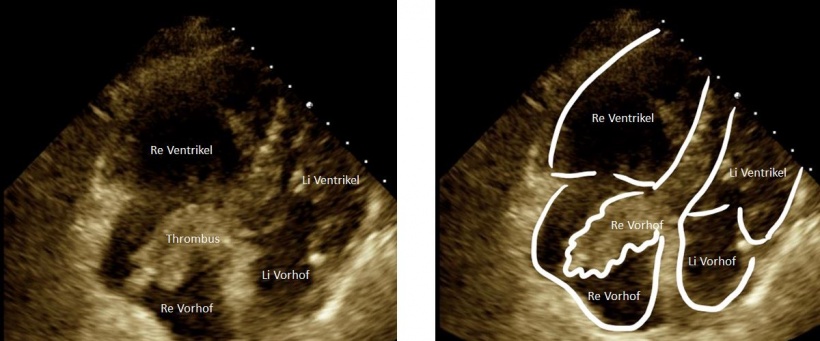
In patients with severe trauma ultrasound can localise the cause of internal bleeding. Even a pericardial tamponade, i.e. bleeding into the pericardium, can quickly be diagnosed with the help of ultrasound. ‘Before ultrasound it was only possible to assume such diagnosis,’ the professor points out. ‘With ultrasound however we can say within 30 seconds whether a patient has a pericardial tamponade, a pneumothorax, blood in the abdomen or the lungs.’
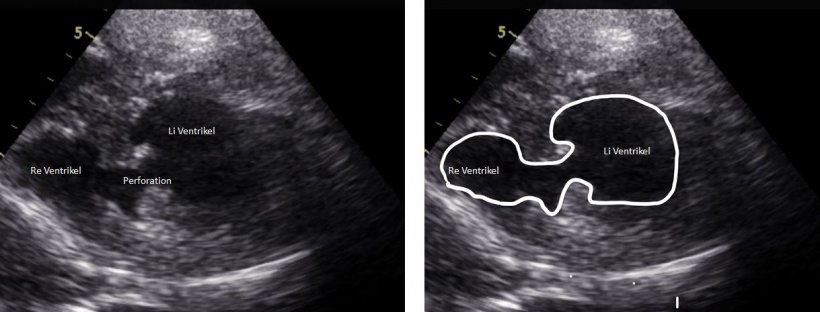
An ultrasound examination in A&E is different from a conventional ultrasound examination. First, it is a focused ultrasound, aimed exclusively at establishing the diagnosis relevant to the emergency situation. ‘For instance, only the appendix is scanned in A&E when appendicitis is suspected. A potential small tumour in the adrenal glands is therefore unlikely to be detected,’ Osterwalder explains. In A&E, the scan is also a POCT-ultrasound, i.e. carried out by the local examining doctor. Last, it is an interdisciplinary examination; with a trauma patient, several different medical disciplines will need to become involved: Is there fluid in the abdomen; fluid around the heart; fluid around the lungs? Is there air in the pleural space (pneumothorax)?
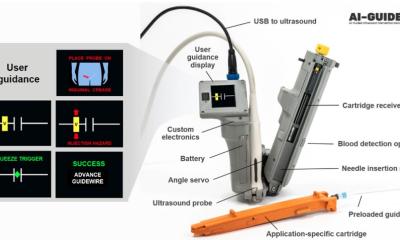
According to Osterwalder, the future lies in personalised ultrasound. This means a doctor carries his/her own ultrasound scanner in their coat pocket. ‘Ultrasound will take over from the stethoscope,’ he is convinced – not only in A&E but also in general practitioner (GP) surgeries and during hospital ward rounds.
In my view, all doctors should be taught the basics of ultrasound during their medical training.
Joseph Osterwalder
Ultrasound transducers of manageable size are now available that can be connected wirelessly to a smartphone or an iPad via an app. ‘There are products on the market already which only cost 2,000 Swiss Francs. Although the image quality they produce is not outstanding it is fairly good, and sufficient for triage,’ he points out. For a patient with back or flank pain, it is easy to establish whether the aorta is enlarged or ruptured, or whether the renal pelvis is distended because of a kidney stone.
‘In my view, all doctors should be taught the basics of ultrasound during their medical training,’ Osterwalder believes. Germany, Austria and Switzerland still have a long way to go, but not the USA, where many medical faculties already teach anatomy with the help of handheld ultrasound transducers. ‘We also have universities here in Switzerland, where students have already taken the initiative to introduce this,’ Osterwalder explains, ‘but the curricula do not yet attach enough importance to ultrasound anatomy.’
Profile:
In April 2017, Swiss accident and emergency specialist Professor Joseph Osterwalder MD FESEM MPH became Medical Director of the Cantonal Hospital in Appenzell, following his leadership, since 1988, of the A&E Department at the Cantonal Hospital St. Gallen. A medical student in Zurich, he completed his habilitation in Geneva, and is now an emeritus professor of the University of Geneva. A member of numerous national and international associations, he has more than 250 publications to his name and runs DEGUM Level III training courses.
14.11.2017