Article • Atrial fibrillation
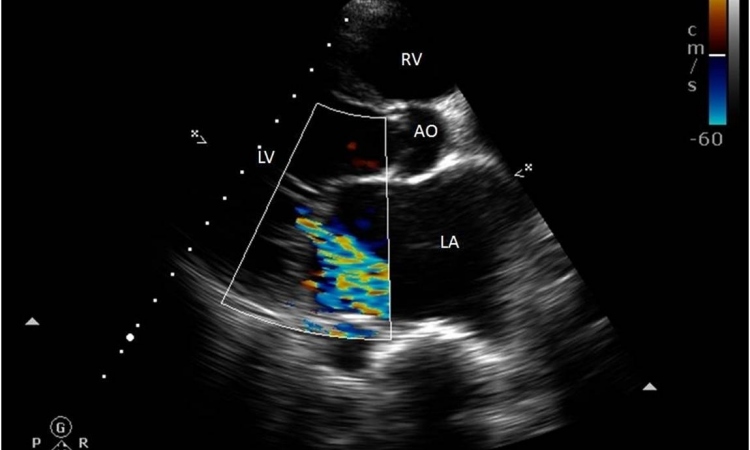
Transthoracic echocardiography
The role transthoracic echocardiography plays in a number of common clinical scenarios was discussed by leading cardiac imaging experts at this year’s British Cardiovascular Society Conference.
Report: Mark Nicholls

Posing the question of when transthoracic echocardiography should be used, four senior figures in cardiac imagery examined its value in atrial fibrillation, chemotherapy, hypertension and stroke.
Speaking in this session, Dr Dipak Kotecha, a clinician scientist in cardiovascular medicine at the University of Birmingham and consultant cardiologist specialising in cardiac imaging, said transthoracic echocardiography had a significant role to play in atrial fibrillation (AF). ‘AF,’ he said, ‘is becoming more prevalent and echo is important and essential in the patient management pathway. Incidence is expected to double in the next 20 years and by 2030 there will be 15-20 million people in Europe with AF. ‘We have to do echo in AF for ejection fraction but it is important for choosing what rhythm control drug you may use or whether it’s safe to use rhythm control in the first place. ‘Echo should be considered for all AF patients, as we are looking for LV function, risk of stroke, safety of rhythm control drugs and interventional support.’

Within hypertension Professor Jamil Mayet – who heads the Surgery, Cardiovascular and Cancer clinical, educational and research programmes at Imperial College Healthcare NHS Trust in London – outlined how transthoracic echocardiography can be used to try to support patients, to decide which ones receive treatment and for risk stratification. He explained that it can be used to assess whether there is left ventricular hypertrophy (LVH), diastolic dysfunction, LV systolic dysfunction, aortic valve issues or to assess myocardial ischemia.
Concluding that transthoracic echocardiography has a role to play in hypertension, he said: ‘With patients who have stage one hypertension, we need to decide whether to treat the risk factors, lifestyle, or with drugs, and we can use echo if we are going to change the management of patients.
‘Patients who will benefit from referral for routine echocardiograph are those with borderline blood pressure, where LVH may have an influence on the decision to treat; possibility of white coat hypertension; risk stratification in patients with multiple risk factors or routine reasons for echo, such as shortness of breath.’

Dr Leonard Shapiro, consultant structural interventionist at Papworth Hospital, Cambridge, suggested that the use of transthoracic echocardiography was not critical in all cases of stroke, but had value if it made a contribution to the management of patients.
Dr Thomas Mathew, consultant cardiologist at Nottingham University Hospitals NHS Trust discussed the role of transthoracic echocardiography in patients undergoing chemotherapy in the context of cardio-toxicity. With patients suffering cellular destruction, biopsy changes, cumulative dose-related effects and permanent damage as a result of chemotherapy, echocardiography had a role in their assessment. ‘We should use the best form of echocardiography available and, on the evidence it is 3-DE as 2-DE fails to detect small changes in contractility. If 2-DE has to be used, it should be with GLS or Troponin, which is the best biomarker in this context.’
Mathew is concerned that all heart failure trials have excluded patients with cancer and there are no proper studies in this evaluation group. ‘Using echocardiography is important,’ he underlined. ‘The main purpose is to decide whether to continue or stop chemotherapy because of the risk.
Profiles:
Dr Thomas Mathew is the clinical lead for cardiac imaging at Nottingham University Hospitals and specialises in echocardiography, cardiovascular magnetic resonance imaging and nuclear cardiology. He is also the training programme director for East Midlands North Deanery and a member of the BCS training committee. An elected council member of the British Society of Echocardiography and a member of the BSE educational committee, he is also an editorial board member of the British Journal of Echocardiography. With more than fifteen years’ experience in cardiovascular imaging, his interests include non-invasive imaging of ischaemic heart disease, valve assessments and cardiomyopathies.
Dr Dipak Kotecha MD is a clinician/scientist in cardiovascular medicine at the University of Birmingham and a Consultant Cardiologist at Queen Elizabeth Hospital, Birmingham, specialising in cardiac imaging. An Honorary Research Fellow at the Royal Brompton Hospital, London, and the Monash University Centre of Cardiovascular Research & Education, Melbourne, he is a Task Force member for the European Society of Cardiology Guidelines on Atrial Fibrillation, and is currently writing the next set of practice guidelines that will be published in 2016. His main research interests are heart failure and atrial fibrillation.
31.08.2015