The role of the immune system in cancer therapy
Apart from tumour immunologists themselves, for a long time oncologists have underestimated the role of the immune system in cancer treatment. Nonetheless, in recent years increasing attention has been given to this aspect of cancer.

One eminent researcher, who has studied the dynamic interactions of tumour cells and the immune system for some time, is Dr Guido Kroemer. In his lecture ‘Immuno-surveillance induced by cytotoxic anticancer agents - a necessary step for therapeutic success’, given at the Max Delbrück Centre for Molecular Medicine in Berlin, he presented his latest discoveries. Bettina Döbereiner spoke with renowned cell death expert about the role of the immune system in cancer therapy.
His findings suggest that some particularly efficient chemotherapeutics can mobilise the host’s immune system against cancer and thus significantly improve cancer treatment. ‘The first results of our studies led us to believe that some conventional cytotoxic chemotherapies agents convert dying cancer cells into a sort of vaccine that stimulates an anti-tumour immune response thereby making therapy more effective,’ said Guido Kroemer, introducing his lecture during Cancer Day at the Max Delbrück Centre for Molecular Medicine, Berlin. He and his team, co-directed by Laurence Zitvogel, could demonstrate in animal experiments with mice that anticancer agents like anthracyclines and oxaliplatines cause an endoplasmic reticulum stress response in cancer cells, resulting in the abnormal cell surface exposure of calreticulin, a protein that normally is hidden within the interior of the cell. Once the immune system has identified calreticulin, it attacks and kills tumour cells of different kinds, including a particular colon cancer cell line (CT 26).
However, this complex response only took place in immune-competent mice, meaning that chemotherapeutic regimes based on anthracyclines or oxaliplatin were less efficient in reducing tumour growth in immune-deficient mice. Moreover, only few of the conventionally used and commercially available chemotherapeutics were able to elicit an anticancer immune response. The reason why some agents cause this so called ‘immunogenic cell death’ is, according to Guido Kroemer, still poorly understood. Even chemically related agents like cisplatin, which works at a first sight exactly in the same way as oxaliplatin, do not cause the calreticulin exposure required for cancer cell death to elicit an immune response.
The role of cardiac glycosides in cancer therapy
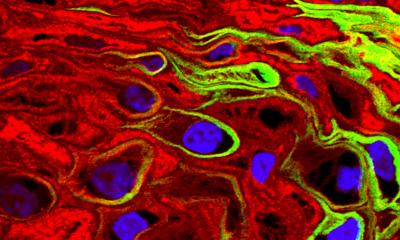
After these first findings Guido Kroemer’s team and Laurence Zitvogel also analysed whether any other drugs, used to treat other diseases, may cause immunogenic cell death in cancer cells. Thus they systematically tested 980 FDA approved drugs by means of a tailor-made fluorescence microscopy platform that allows for the automated detection of the biochemical hallmarks of immunogenic cell death. This approach led to the unexpected finding that several cardiac glycosides (CG) were among the most efficient inducers of the hallmarks of immunogenic cell death including calreticulin exposure. Cardiac glycosides, which include the components of the foxglove plant (digitalis) digoxin and digitoxin, have been used for many years for the treatment of heart failure and atrial arrhythmia.
Animal models: Cardiac glycosides induce immunogenic cell death of cancer cells
Although it is not new that CGs might have some positive impact on cancer – the first epidemiological report on the anticancer effects of CGs was published in 1982 by Björn Stenkvist – these new findings help to understand the mechanisms accounting for their anticancer effects, an effect that implies the induction of immunogenic cell death of cancer cells. Indeed, CGs could enhance the anticancer effect of drugs that alone are unable to induce immunogenic cell death, such as cisplatin, but only in immune-competent mice. The combined anticancer effect of CGs plus cisplatin was lost in immuno-deficient mice, demonstrating that it was immune-dependent. Confirming these results, the researchers could also show that cancer cells succumbing to a combination of cisplatin plus cardiac glycosides could vaccinate syngeneic mice against a subsequent challenge with live cells of the same type.
Retrospective analysis showed effect of CGs in humans
Finally, Guido Kroemer and team analysed 435 computerised patient files from the Institut Gustave Roussy in a retrospective clinical study that was designed to determine, whether CG interact positively with chemotherapy. This study revealed that the administration of the cardiac glycoside digoxin during conventional cancer therapy, mostly chemotherapy or radiotherapy had a positive impact on overall survival in cohorts of breast, colorectal, head and neck, and hepatocellular carcinoma patients. ‘We expected, of course, that patients affected by an underlying cardiopathy, arrhythmia or heart insufficiency, would die well before the control group, but we found the contrary. The overall survival of digoxin-treated patients was better than that of the control group.’ This is not true for lung cancer and prostate cancer, as Guido Kroemer added. ‘Perhaps because chemotherapy in the lung does not work anyway and because prostate cancer is mostly treated by chemical castration, not by chemotherapy.’
The results also revealed – as well as in the mentioned animal model –that cardiac glycosides only interact positively with chemotherapeutic agents that, given as mono-therapies fail to induce immunogenic cell death like, for example cisplatin. Therefore only this kind of per se non-immunogenic chemotherapy could be improved by cardiac glycosides. Guido Kroemer and Laurence Zitvogel are currently launching a clinical trial that will evaluated whether co-medication with digoxin may improve the current standard of care of locally advanced head-and-neck cancer, which are normally treated with cisplatin-based chemotherapy and radiotherapy.
Consequences for future research
Based on these results, which suggest a hitherto unexpected link between the success of chemotherapy and the immune system, Guido Kroemer proposed a new organisation of drug development and approval. He argued that most scientists still conceive cancer as a cell-autonomous disease, yet ignore the essential contribution of immuno-surveillance towards the cure of malignant diseases. This would lead to the premature launching of clinical trials that finally turn out unsuccessful. ‘We should introduce a filter during pre-clinical evaluation to prevent the high attrition-rate of over 95 percent in clinical trials’ he claimed.
Thus he proposed that, after identifying an agent that has some effects on tumour cells in vitro, the agent should be analysed with regard to its potential to induce immunogenic cell death or other positive effects on the immune system. ‘Only once an agent has been tested in immuno-competent mouse models and has turned out to mediate satisfactory immuno-stimulatory effects, should it be introduced into clinical trials. Through this procedure,’ he said, ‘scientists would select immune-stimulatory molecules in mice before clinicians do so in patients’.
PROFILE:
In 1995, after gaining MD and PhD degrees at Innsbruck University, Austria, Guido Kroemer undertook post-doctoral training at the Collège de France, Nogent-sur-Marne. He was also awarded a doctorate in biology at the Autonomous University of Madrid in 1992, where he worked as a group leader at the National Centre of Molecular Biology (1990-1992) and at the National Centre of Biotechnology (1993). He later joined various research teams at the French National Institute of Health and Medical Research (INSERM).
Since 2007, he has directed the INSERM unit 848, covering research on apoptosis, cancer and immunity at the Institut Gustave Roussy near Paris.
Worldwide, Dr Kroemer is one of the most cited cell death scientists. Besides many honours and awards, he received in 2006 the Descartes Prize, the EU’s highest scientific distinction, for his fundamental discoveries in apoptosis.
29.07.2013