Fibrocartilage
Structure to aid better replacements and injury treatments
Fibrocartilage tissue in the knee is comprised of a more varied molecular structure than researchers previously appreciated, according to a new study by researchers from the Perelman School of Medicine at the University of Pennsylvania and the University of Delaware.
Their work informs ways to better treat such injuries as knee meniscus tears - treatment of which are the most common orthopaedic surgery in the United States -- and age-related tissue degeneration, both of which can have significant socioeconomic and quality-of-life costs. The team published their work this week online ahead of print in Nature Materials.
The development of effective treatment strategies to address injuries to the body's load-bearing tissues has been hindered by a lack of understanding of the interplay between structure and function and how cells within these specialized tissues respond to mechanical inputs, such as walking, running, and physical activity. Without this information, discovery, and development of effective treatment strategies to ameliorate these conditions has been held back. While tissue-engineered models exist that can mimic various aspects of healthy natural tissue structure and function, these do not simulate early tissue degeneration and its effect on structure, mechanical properties, and cell biology.
"To be able to probe natural tissue structure-function relationships, we developed micro-engineered models to advance our understanding of tissue development, homeostasis, degeneration, and regeneration in a more controlled manner," said co-senior author Robert L. Mauck, PhD, an associate professor of Orthopaedic Surgery and Bioengineering at Penn. "Our tissue-engineered constructs match the structural, mechanical, and biological properties of native tissue during the process of tissue formation and degeneration. Essentially, we are working to engineer tissues not just to provide healthy replacements, but also to better understand what is happening to cause degeneration in the first place."
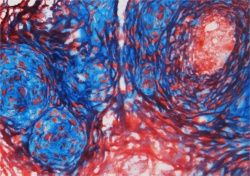
The team describes that the meniscus tissues of knees are comprised of fibrous regions consisting of long, aligned fibers that give the tissue strength and stiffness. However, within this fibrous region are small non-fibrous regions called microdomains that have a different composition, with concomitant different mechanical properties. While the aligned fibrous regions transmit mechanical deformation signals directly to surrounding cells, the proteoglycan-rich microdomains do not deform at all.
"Our first question when we saw these microdomains was "'Are they normal, or are they associated with pathology?'" asked co senior author Dawn Elliott, PhD, professor and chair of Delaware's department of Biomedical Engineering.
Studies performed in the Elliott lab using cow and donated human tissue showed that microdomains are present in very young healthy tissue, but these microdomains grew larger with age, injury, and such disorders as osteoarthritis, suggesting that increased microdomain size is related to disease onset and loss of tissue function.
The team surmised that cells in the fibrous regions and proteoglycan rich microdomains were not receiving the same mechanical signals. In fact, the cells within the microdomains did not respond to mechanical inputs, while cells in the fibrous regions switched calcium signals on and off in response to mechanical loading. These cells likely sensed the physical inputs when stretched - similar to stresses on muscles when exercising -- and converted the mechanical input into a biochemical message, in this case calcium flow through the cell membrane.
Mauck next developed a tissue engineered model to better control variables compared to natural tissue. His lab devised a micro-scaled culture platform to generate engineered tissue with both normal and abnormal features and looked at differences in physical structure and cell signaling in response to mechanical loading. These engineered microtissues replicated the key features of degenerating native tissue and can now serve as a platform for testing new treatment strategies, whether physical in nature -- such as physical therapy -- or drug-based.
"This engineered disease model will enable the development of new treatments for degenerative disease in numerous types of connective tissues," Mauck said.
Source: University of Pennsylvania School of Medicine
12.01.2016





