Röntgen Prize for Marc Dewey
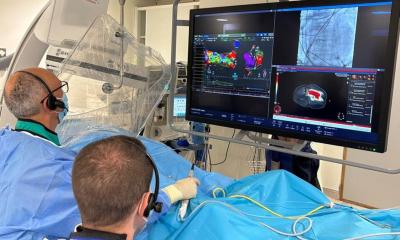
Berlin-based radiologist Marc Dewey will be awarded this year's Röntgen Prize for his work on the diagnosis of coronary heart diseases (CHD), one of most common and most dangerous heart conditions in the industrialized countries.

Dr Dewey was able to show that non-invasive computed tomography is frequently equally suited to detect the plaque that builds up on the inside of the heart arteries as invasive catheters. “In Germany alone, approximately 700,000 catherizations are performed each year, most of them for purely diagnostic purposes. Our studies have shown that CT images visualize treatment-relevant stenoses as well as heart catheterization does, an invasive procedure which is not free of risks”, explains Dr Dewey. Patient satisfaction is another important issue, he adds: “We surveyed patients who had undergone both CT and catherization and found out that two thirds preferred the pain-free CT diagnosis.”
Below you can read an interview with Dr Dewey on this issue published in European Hospital earlier.
Although cardiac catheterisation is considered the current gold standard for coronary artery disease (CAD) diagnosis, a new cost-effectiveness model* indicates that, in many cases, a CT coronary angiography (CTCA) not only provides a better diagnostic outcome but is also cheaper. Meike Lerner discussed the implications of the study and his cost-effectiveness model with Dr Marc Dewey, of the Radiology Institute at Charité University of Medicine – Berlin
‘Our model is based on clinical studies regarding the sensitivity and specificity of the different diagnostic methods: cardiac catheterisation, coronary angiography and calcium scoring, using CT as well as stress MRI with dobutamine,’ Dr Dewey explained. ‘This means, we did not perform clinical studies ourselves but analysed published data on the accuracy of these methods.
Consequently, our calculation has to be verified in practice. More so since our model is based on one crucial practical aspect: a thorough medical history taken by a physician. In the end, the effectiveness of a method depends to a large extent on the pre-test probability – the assessment of the probability of a disease according to certain clinical parameters. Indeed, from a cost-effectiveness point of view, not all patients are suited for a CTCA.
‘Rather the results of our cost-effectiveness analysis indicate that in patients with a pre-test probability of over 60% a CTCA does not make sense. This holds true not only from an economic point of view but above all from a medical point of view, since, in patients with a high pre-test probability, the likelihood of a treatment increases – and the likelihood that the treatment can be performed with a heart catheter. Moreover, patients with a high pre-test CAD probability cannot be safely ruled out to have disease with non-invasive tests. Almost always, this group shows positive results, consequently those patients have to undergo catheterisation anyway. Unfortunately, current common practice is that, for example, patients with a 70% pre-test probability first undergo a non-invasive test – only to find out what was to be expected: the patient requires catheterisation. That obviously generates additional costs.
When is a CTCA recommended?
‘About a third to 50% of symptomatic patients have a pre-test probability of less than 50–60%. This means CAD can be reliably excluded with a CT examination. Due to the high sensitivity of this method, the rate of false diagnoses is below 10%. Therefore, from a cost-effectiveness point of view, patients with a low pre-test probability – less than 60% – should not undergo cardiac catheterisation. This is also clinical practice: an immediate invasive approach is avoided for those patients. Nevertheless: according to a study, two thirds of all cardiac catheterisations in Germany do not lead to immediate therapeutic consequences. This is reason enough to reconsider. Fortunately, in other European countries the figures are not as extreme. Scandinavian countries, the Netherlands and Great Britain have significantly fewer superfluous heart catheterisations. These are countries where the state has quite a say in the healthcare system and where the financial interests of the actors in the healthcare system are not as intense – that is, reimbursement is not based on the type and number of examinations.
‘We hope our model can raise awareness of this fact and help focus on non-invasive gentle methods that have medical and economic advantages for patients with low to intermediate pre-test probability.’
Despite all the advantages, a CT examination means radiation exposure. Does your model indicate that MRI is a viable option?
‘Obviously we don’t want to ignore the (albeit minor) risk associated with radiation exposure – but that risk is comparable to that of cardiac catheterisation. However, the situation is quite different as soon as you have double tests: CT and catheter. In terms of cost-effectiveness, the advantage of CT is its accuracy compared with stress echocardiography, stress ECG and MRI coronary angiography. CT sensitivity is above 90%, that of MRI coronary angiography is just above 70%. In our cost-effectiveness model we looked at stress MRI. This type of examination is more accurate – it has an over 80% sensitivity – but it is neither accurate nor cheap enough to be considered more cost-effective than a CT. Moreover, as the name says, stress MRI means exposing the patient during the CAD diagnosis to a certain degree of stress. However, MRI is very useful to analyse myocardial viability – a crucial aspect for the further management of patients with known CAD. For this purpose, MRI is more accurate than other methods, such as myocardial scintigraphy.’
Would you make specific clinical recommendations based on the results of your model?
‘To make certain clinical recommendations based on a cost-effectiveness model is rather difficult. Obviously our data are culled from studies on sensitivity and specificity, but we have not yet applied our models in practice, respectively in studies. As long as we do not have such real-life results, we cannot say whether our model is clinically useful. In real life, there are always a number of components that interact, such as workflow in hospitals, or between them and physicians’ offices. In our opinion we clearly need a study on how CT-based diagnosis will influence therapeutic management. This would provide a basis on which general recommendations might be formulated. However, our model does show that, from a cost-effectiveness point of view, CT is superior to other diagnostic procedures for patients with a pre-test probability of up to 60%.
Another crucial question is: Who benefits from cost-effectiveness calculations? Our model looks at CAD diagnosis from the standpoint of society as a whole. To put it simply: We asked how much money can society save in terms of health insurance premiums and related expenses by optimising diagnostic management? The hospitals themselves look at CAD diagnosis from a very different angle: unfortunately, they make more money with invasive procedures because the DRG system offers higher reimbursement rates and thus higher profits for invasive procedures.
With regard to Germany, we also analysed how useful CTCA is from the perspective of office-based radiologists. For them the situation is quite different than for hospitals: current reimbursement rates for CT examinations do not cover their expenses and, even in the long run, they will not be able to reach a break even point. Consequently, office-based radiologists have little interest in implementing our model if it is not accompanied by an increase in reimbursement rates. However, according to our analysis, an increase of the net reimbursement for radiologists of about 75% means the radiologist can reach break even and CTCA still remains the most cost-effective method from society’s perspective. We hope this is a convincing argument to increase CT reimbursement rates. For this to happen, however, certain preconditions must be created. As long as this does not happen, our model will remain a theoretical approach. Nevertheless, we consider our cost effectiveness analysis a suitable basis for further optimisation of both diagnostics and management of patients with suspected coronary artery disease.
* Cost effectiveness of coronary angiography and calcium scoring using CT and stress MRI for diagnosis of coronary artery disease. Marc Dewey; Bernd Hamm, Eur Radiol DOI 10.1007/s00330-006-0439-3
26.05.2009