News • video-assisted thoracoscopic
Revolutionary surgery for lung cancer
The University of Montreal Hospital Research Centre (CRCHUM) is launching a major international clinical trial to test a minimally invasive and safer surgical approach for patients with lung cancer: video-assisted thoracoscopic (VATS) lobectomy with ultrasonic pulmonary artery sealing.
I think this technique could completely change the way we perform surgery for lung cancer, which is the deadliest form of cancer in North America.
Dr. Moishe Liberman
The University of Montreal Hospital Research Centre (CRCHUM) is launching a major international clinical trial to test a minimally invasive and safer surgical approach for patients with lung cancer: video-assisted thoracoscopic (VATS) lobectomy with ultrasonic pulmonary artery sealing.
Monic Ste-Marie, 48, is one of the first to benefit from this procedure developed by Dr. Moishe Liberman, a thoracic surgeon and researcher at the CRCHUM. On January 19, 2016, he successfully removed the one-centimetre tumour lodged in her left lung. The operation involved making three small incisions in her chest and then removing the diseased portion of her lung, guided by a video camera and using an electronic device to seal the pulmonary artery by ultrasound to prevent bleeding during the operation.
“I think this technique could completely change the way we perform surgery for lung cancer, which is the deadliest form of cancer in North America," said Dr. Liberman, who is also an Associate Professor of Surgery at the University of Montreal.
Currently, pulmonary lobectomy is the most commonly performed lung cancer operation in the world. It involves opening the chest and cutting the ribs to remove the lung lobe containing the cancerous tumour. But it leaves a long scar, and patients take up to six months to recover from this invasive and risky procedure. In the past 20 years, a new technique has developed: video-assisted thoracoscopic (VATS) lobectomy. Instead of making a long incision in the chest and breaking the ribs, surgeons simply make small holes to reach the target area. Their actions are guided by a miniature video camera inserted in the chest wall through one of the holes.
“The technique is beneficial, but it is not widely practiced, because the risk of major bleeding makes it difficult to control. Pulmonary arteries are thin and fragile. If there is bleeding during open surgery then it’s easy: we stitch it up and that’s it. But when we work with a camera and there is bleeding and we can’t see through the lens, the patient can die quickly, because the pulmonary artery is connected directly to the heart,” explained Dr. Liberman.
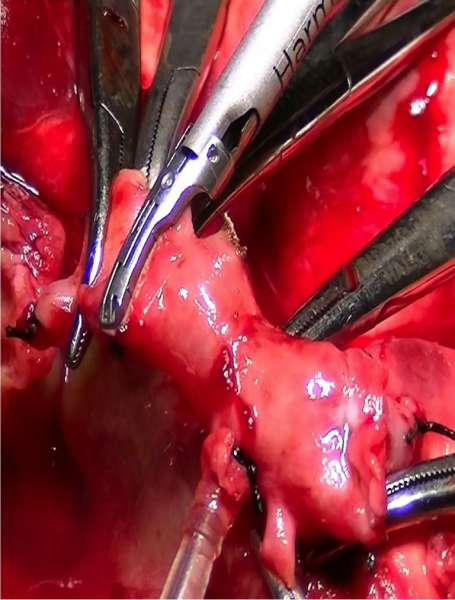
To facilitate and secure the procedure, he uses a new tool: a kind of pistol with a small three-millimetre jaw at the end that seals the blood vessels using ultrasonic energy. The device, called the HARMONIC ACE®+7 Shears was designed by Ethicon, part of Johnson & Johnson. It is commonly used to seal small blood vessels under seven mm in diameter. Dr. Liberman hopes to demonstrate that the ultrasound gun is also effective for pulmonary artery branches.
After five years of pre-clinical studies at the CRCHUM, first with animals and then in Phase 1 and 2 clinical trials that demonstrated the safety of the procedure, Dr. Liberman is now leading a large multi-centre Phase 2 clinical to assess the effectiveness of the technique in 150 patients in Canada, the US, and Europe. The $1.8 million project is funded by Johnson & Johnson. The results should be available in four years.
Each year, lung cancer kills around 1.59 million people in the world, largely due to smoking, which is responsible for 80% of cases, according to the World Health Organization. The cancer is particularly alarming because it is often diagnosed late, and the survival rate five years after diagnosis is rather low: 17% in women and 14% men.
Dr. Liberman hopes the new surgical approach he developed will save lives. "I think it will decrease the risk of bleeding and reduce post-operative pain. Patients will be able to resume their normal lives more quickly,” he said. Monic Ste-Marie was fortunate. Her lung cancer was diagnosed quickly. Six months after the pioneering medical procedure that saved her life, she is doing well: “I had pain for a month after the operation. Now, I still have trouble catching my breath, but that’s normal,” she said.
Source: Universite de Montreal
15.07.2016





