Image source: RCI
News • Regenerative properties discovered
Reprogramming immune cells to repair tissue damage
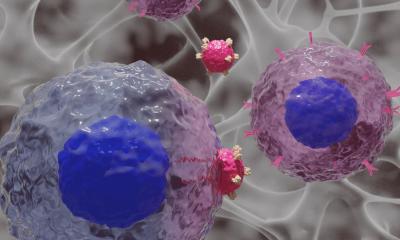
Regulatory T cells (Treg cells) are an immune cell type that reduces excessive immune responses and protects the body against autoimmune diseases. A new study shows that Treg cells in human tissues acquire tissue-regenerative features and describes a method to generate these cells in the laboratory.
The immune system’s main function is to defend the body against infections or cancer. In recent years, investigations in mice revealed that immune cells also have the important role of supporting the healing of damaged tissues and of maintaining the normal function of healthy tissues. One type of immune cells with particularly strong tissue-regenerative features are the regulatory T (Treg) cells. Former studies in mice have revealed an important role of these cells in promoting tissue regeneration in virus induced lung damage, stroke, colitis, muscle repair and metabolic disorders. However, it remained so far unclear whether the human immune system has comparable capacities. Scientists at the Regensburg Center for Interventional Immunology (RCI) have now identified and characterized human tissue-regenerative Treg cells. They also developed a manufacturing method to generate these cells in the lab, opening up the possibility of using these cells for regenerative medicine. These findings are now published in the journal Immunity.
We might be able to use these cells to repair tissue damage after bone marrow transplantation, a treatment to combat leukemia and other blood cancers
Markus Feuerer
Michael Delacher, Ph.D. and Markus Feuerer, M.D, from the RCI built on their previous studies in which they described tissue-regenerative Treg cells in mice[1], [2] and elucidated their developmental pathway[3].
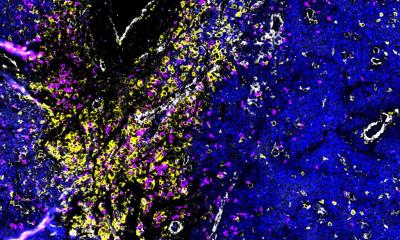
Cells determine all their features and functions through “on” and “off” switches that are distributed over the entire genome and regulate the activity of each gene. Together these form an “epigenetic fingerprint” which is highly specific for a particular cell type. By comparing the epigenetic fingerprints of tissue resident Treg cells in humans and mice the scientists identified a species-conserved tissue-regenerative Treg signature. “This epigenetic signature combined with gene expression profiling enabled us to pinpoint the exact nature of human tissue-regenerative Treg cells.” said Delacher. “We found that tissue-regenerative Treg cells share several features with another type of T cells – the so-called T follicular helper (Tfh)- a cell subset that orchestrates the production of antibodies.” noted Malte Simon, a bioinformatician from the German Cancer Research Center, who was involved in bioinformatic analysis of this study. This observation turned out to be critical for the development of a manufacturing protocol for tissue-regenerative Treg cells. “Since culture conditions promoting the generation of Tfh-like cells were previously known, we adopted them for the manufacturing of tissue-regenerative Treg cells”, said Lieke Sanderink, a PhD student at the RCI involved in the programming of Treg cells.
On this basis, the RCI scientists plan to design specific cell therapies employing tissue-regenerative Treg cells for regenerative medicine. “We might be able to use these cells to repair tissue damage after bone marrow transplantation, a treatment to combat leukemia and other blood cancers” said Feuerer.
A dark side of tissue-regenerative Treg cells is their support of tumor growth. “Once we better understand how these cells activate their functions we may be able to inhibit their counterproductive effects in tumors to enhance the success of cancer treatment” said Philipp Beckhove, the RCI scientific director.
References:
[1] Delacher M, et al. Genome-wide DNA-methylation landscape defines specialization of regulatory T cells in tissues. Nature Immunology, 2017; 18(10):1160-1172
[2] Delacher M, et al. RBPJ expression in regulatory T cells is critical for restraining TH2 responses. Nature Communications, 2019; 10(1):1621
[3] Delacher M, et al. Precursors for Nonlymphoid-Tissue Treg Cells Reside in Secondary Lymphoid Organs and Are Programmed by the Transcription Factor BATF. Immunity, 2020; 18;52(2):295-312
Source: University Hospital Regensburg
01.04.2021