Using MRI scans
Refining the criteria used to diagnose MS at an early stage
The 32nd Congress of the European Committee for Treatment and Research in Multiple Sclerosis opened in London (September 14-17) and key presentations reveal the latest evidence-based thinking on how to use MRI scan results to diagnose MS with increasing accuracy. Earlier this year, MAGNIMS, the European Collaborative Research Network that studies the use of MRI when diagnosing MS, published revised criteria for clinicians.[i]
In his presentation at ECTRIMS, Paolo Preziosa (Vita-Salute San Raffaele University, Milan, Italy) a young investigator within MAGNIMS, outlined results showing that their most recent techniques do indeed make it possible to diagnose MS earlier and more accurately in patients with very few clinical signs of the disease.
Using MRI data in MS diagnosis requires continual reassessment
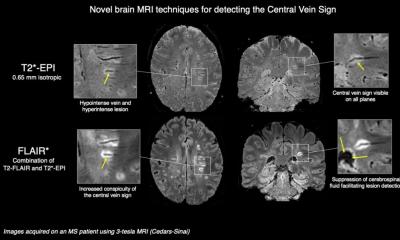
MRI scans have been used routinely to help diagnose MS since 2001. Over the last 15 years there have been huge advances in the technology and so the criteria used to diagnose MS in patients on the basis of their scans results have had to change too.
One of the key goals is to use MRI imaging to detect changes within the brain and spinal cord of someone who has Clinically Isolated Syndrome (CIS). This term is used to describe someone who has experienced a single episode of neurological symptoms. This episode may have lasted only a few days, leaving clinicians with very little to go on when attempting to determine the underlying cause.
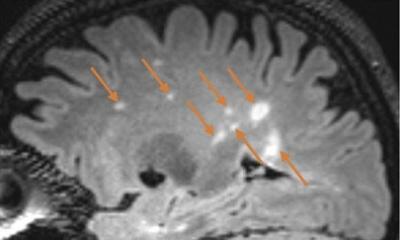
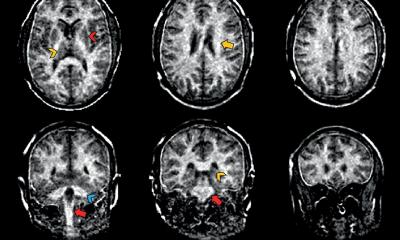
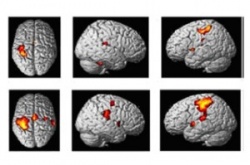
One of the key factors that MRI data is used to look for is whether the symptoms are caused by lesions in the nervous system that are ‘disseminated in time and space’. Using MRI technology to judge whether abnormalities in the grey matter particularly are associated with a subtle spread and progression of the disease is at the heart of the recent criteria.
Defining the criteria for a diagnosis of MS
Preziosa explained that the new criteria for MS diagnosis in patients with CIS specify that at least two of the following signs are visible on a detailed MRI scan:
- At least one lesion in the spinal cord
- Three or more lesions in the periventricular white matter in the brain
- At least one lesion in the infratentorial region, which includes the cerebellum
- At least one lesion in the cortical or juxtacortical region of the brain – so in or near the grey matter
- At least one lesion in an optic nerve
Preziosa emphasized that scoring cortical lesions (the grey matter) and lesions involving the white matter next to the cortex (called juxtacortical lesions) when assessing ‘dissemination in space’ was a key change to the current criteria and one that required detailed investigation within a clinical study.
The MAGNIMS study to test out the new criteria
During their work on the recent consensus statements, the MAGNIMS group set up a study involving 72 patients with CIS who were recruited from five European centres and followed up for over 2 years. One of the objectives was to reveal better the lesions present in the grey matter and in the adjacent white matter. Finding lesions in or near the grey matter can be particularly difficult: Preziosa explained that patients in the study had a double inversion recovery MRI (DIR MRI) scan at study entry as this increases grey matter lesion detection compared to standard MRI.
After two years, 90% of those recruited to the study had developed MS, while 10% were found to have a separate neurological condition. Encouragingly, the use of DIR MRI to detect lesions in the grey matter led to more patients being correctly diagnosed with MS right at the start of the study. The group concludes that the changes that they have proposed to the diagnostic criteria for MS do indeed make it possible to diagnose MS in someone with very early clinical symptoms much more accurately.
Prof. David Miller, Vice President & Chair of Scientific Committee of ECTRIMS: “These refinements in criteria seem to be small steps, but for patients with early stage MS, they are very significant. Being able to give someone an accurate diagnosis of MS enables disease-modifying treatments to be given as early as possible. Equally, if someone does not have MS, their clinical team can then move forward to finding out what is the cause of their symptoms.”
Source: European Committee for Treatment and Research in Multiple
[i] Filippi M, Rocca MA, Ciccarelli O, De Stefano N, Evangelou N, Kappos L, et al. MRI criteria for the diagnosis of multiple sclerosis: MAGNIMS consensus guidelines. Lancet Neurol. 2016 Mar;15(3):292-303. doi: 10.1016/S1474-4422(15)00393-2. Epub 2016 Jan 26.
15.09.2016