Source: Cedars-Sinai
News • Neuroimaging
A clearer picture of Multiple Sclerosis
Cedars-Sinai physician-scientists are pioneering imaging techniques and investigating new biomarkers to improve multiple sclerosis (MS) diagnosis and treatment.
Using advanced techniques for imaging the brain and eyes, along with new biomarkers, researchers in the Department of Neurology at Cedars-Sinai are working to present a clearer picture of multiple sclerosis. Their work could lead to improved diagnosis and treatment of the disease, in which the body’s immune system attacks the brain, spinal cord and optic nerves.
“Multiple sclerosis is a disease that can look very different in different people, and the path to diagnosis is equally varied,” said MS specialist Marwa Kaisey, MD, assistant professor of Neurology at Cedars-Sinai. “Diagnosis is complex because many other diseases mimic MS, and while we have a set of diagnostic criteria, there’s no single test that is definitive.”
Misdiagnosis is common
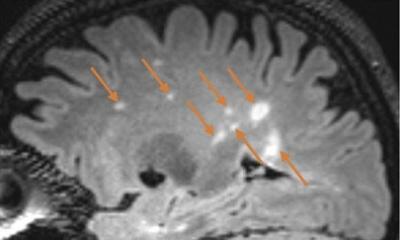
The immune system in patients with MS attacks the insulating layer that protects nerves. The disruption or loss of these layers results in lesions, which show up as white spots on MRI brain scans—the main tool for diagnosing the condition.
MS lesions disrupt communication within the brain and between the brain and other parts of the body, resulting in vision problems and eye pain, double vision, muscle weakness, trouble with coordination, fatigue, dizziness, and hearing and speech problems. But MS is not the only condition that can cause white spots to appear on an MRI. “Almost 1 in 5 new patients coming into our clinic with an existing diagnosis of MS turned out not to actually have MS, according to a study that we published in 2019,” Kaisey said. “When we talk to other MS specialists about this, they're not surprised. They also see this trend of misdiagnosis.”
Kaisey said migraines are the most common cause of non-MS white spots on MRIs. “However, in our past study, among 43 people who were misdiagnosed with MS, we found as many as 27 different conditions actually causing the white spots on their imaging,” Kaisey said.
Patients who are misdiagnosed with MS are needlessly prescribed costly immune-modifying treatments that can increase risk for infection, cause organ damage and decrease the effectiveness of vaccines. “If you have MS, the medications are worth the side effects because they are saving your life and protecting your brain,” Kaisey said. “But it’s a big deal to be on these medications if you don’t need to be.”
New brain signs
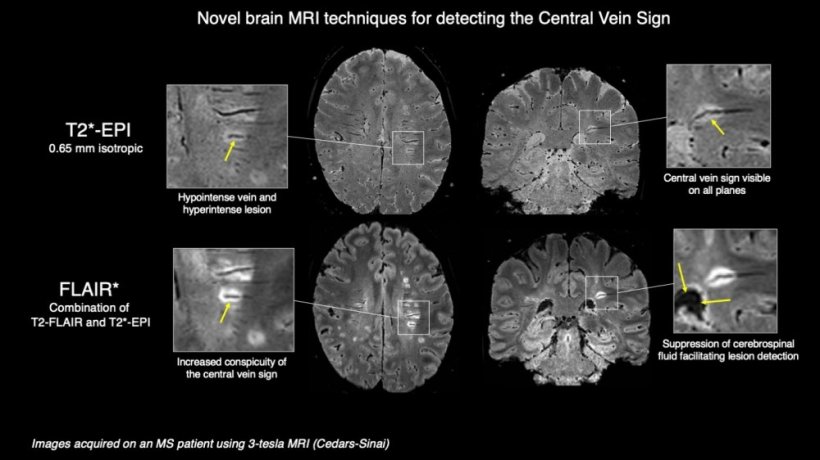
A newly identified biological sign called “central vein sign” could help physicians determine whether white spots on a patient’s MRI are caused by MS or by something else, ultimately reducing misdiagnosis. MS lesions tend to form around tiny veins through which immune cells enter and attack brain tissue, so most lesions caused by MS have a vein in the middle. “We’ve known this for more than 100 years, but until recently we didn’t have a way to see it on an MRI,” Kaisey said.
New MRI techniques pioneered by Pascal Sati, PhD, director of the Neuroimaging Program in the Department of Neurology and associate professor of Neurology at Cedars-Sinai, make central vein sign visible. “Current MRI images don’t give us the whole picture, which is why we developed MRI sequences that improve image quality so that we can see very small veins, called veinules, in the brain,” said Sati. “We superimpose that over a conventional MRI image of the lesions so that it is clear which brain lesions have a central vein and are likely caused by MS.”
Ongoing studies at Cedars-Sinai and 10 other MS centers in North America are using Sati’s technique to image 400 patients at risk of developing MS—the final step in scientifically validating central vein sign as a way to diagnose MS.
Importantly, the imaging technique Sati developed can be used with widely available MRI scanners and performed quickly enough to fit the workflow of the typical radiology center. He is also developing a machine learning algorithm to make evaluation of the imaging results easier for physicians.
“Once the image is taken, our deep learning algorithm can analyze it very quickly and tell the clinician how many lesions show the central vein sign,” Sati said. “The number of lesions with the central vein sign can indicate whether or not the patient has MS.”
The central vein sign could also help doctors determine how well a patient is responding to treatment by confirming that any new lesions that develop are caused by MS and not something else. “With the central vein sign, we can clearly see which lesions are related to MS,” Sati said. “This information is empowering doctors to make decisions about whether to continue a patient’s current therapy, switch to a different MS therapy, or treat them for a completely new, or different, condition.”
Another window into MS
Imaging of the retina—the layer of tissue at the back of the eye—and the optic nerve can also help improve MS diagnosis. Neurologist Omar Al-Louzi, MD, director of the Visual Outcomes Laboratory at Cedars-Sinai, is at the forefront of this technology.
“Around 25% of MS patients experience vision loss or blurring as their first symptom, and as many as 80% experience vision problems at some point in the course of their disease,” said Nancy Sicotte, MD, chair of the Department of Neurology, director of the Multiple Sclerosis and Neuroimmunology Program and Women’s Guild Distinguished Chair in Neurology. “Dr. Al-Louzi’s research seeks to use the eye as a window to produce better outcomes for patients.”
Using a technology called optical coherence tomography (OCT), which functions like an MRI for the retina and optic nerve, Al-Louzi can detect MS lesions that an MRI can miss. “The optic nerves are very small and difficult to image,” Al-Louzi said. “Detecting lesions there can help us clinch an MS diagnosis, especially in patients who are relatively early on in their disease course.”
Optical coherence tomography captures 3D images of patients’ retinal layers, including the ganglion cell layer, which sends visual information to the brain. “Shrinking of the ganglion cell layer often mirrors overall brain degeneration, and occurs in 70% to 80% of MS patients,” Al-Louzi said. “This is why ganglion imaging could also help us improve diagnosis.”
Retinal imaging could also help indicate how well a patient is responding to treatment.
Al-Louzi is continuing to study the role of OCT, along with a related technique called optical coherence tomography angiography (OCTA), as a way to understand how MS affects the blood vessels in the retina. “Our lab is collaborating with Dr. Kaisey to compare the vascular fingerprint of MS in the retina to that of other brain conditions involving blood vessels, such as migraine or small vessel disease, to see whether retinal vessels can help us distinguish between these different conditions,” Al-Louzi said.
While ocular nerve and retinal imaging is important to evaluate in MS patients, it is not yet widely available in practice. Al-Louzi hopes his research will help change the standard of diagnostic care. “I think failing to use these imaging techniques is a missed opportunity,” said Al-Louzi. “Our hope is that these tests will become widespread and shorten the time between symptom onset and getting the right diagnosis.”
Seeing patients wrongly diagnosed with MS, and MS patients who have gone undiagnosed, drives these physicians to keep working toward better solutions. “I didn’t really intend to go into this line of research, but being in clinic every day and seeing these problems firsthand, I just had to do something about them,” Kaisey said. “Almost 1 million people in the U.S. alone live with MS. Fortunately, these imaging techniques could offer an invaluable solution.”
Source: Cedars-Sinai
22.04.2022