© Rick van Rijn
Article • Paediatric trauma in diagnostic imaging
‘It only takes one radiologist to stop child abuse’
Covid-19 has intensified domestic violence rates worldwide, with children among the most vulnerable victims. At the ECR 2025 radiology congress in Vienna, Dr Rick R. Van Rijn presented compelling insights into how radiologists can identify non-accidental trauma (NAT) in children through systematic imaging approaches. From comprehensive skeletal surveys to specific neurological imaging protocols, the expert explained how these techniques are essential for early intervention and potentially life-saving outcomes.
Article: Tim Hofmann
The WHO reports that six out of ten children under age five – approximately 400 million worldwide – regularly experience violence from parents or caregivers. In Europe alone, one in 30 children suffers abuse. Van Rijn, a paediatric radiologist at the Amsterdam University Medical Center (UMC), highlighted that child abuse, particularly abusive head trauma, is a major contributor to fatalities, disabilities, and developmental challenges.1 However, he pointed out that many hospitals still do not have consistent procedures in place for addressing suspected cases.
Europe's guideline, “The Radiological Investigation of Suspected Physical Abuse in Children,” establishes a gold standard for best practices. However, it sets demanding criteria, such as requiring forensically trained radiographers – a standard that remains hard to obtain in many countries. ‘What any radiologist can do, regardless of specialization, is ensure radiographs are of sufficient quality for expert review,’ Van Rijn advised.
Recognizing red flags
First of all, it is important to recognise possible signs of abuse. The "TEN-4-FACESp" rule provides radiologists with a systematic approach to identifying suspicious bruising.
TEN-4-FACESp stands for bruising to the Torso, Ears, Neck, Frenulum, Angle of the jaw, Cheeks, Eyelids or Subconjunctivae, “4” represents infants four months and younger with any bruise, anywhere, and “p” means the presence of patterned bruising. ‘Any of these signs should immediately raise concerns,’ Van Rijn stated. He recounted a tragic case where medical professionals dismissed unexplained bruising in an infant who later died from abuse, underscoring the life-or-death importance of vigilance.
Inconsistencies in reported history provide another crucial warning sign. ‘When parents claim a 4-month-old walked and fell, that's immediately suspicious since children typically begin walking around eleven months,’ he explained.
Comprehensive imaging: the critical first step
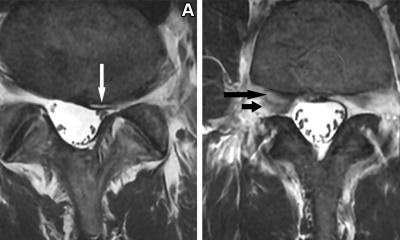
A proper skeletal survey requires 35 radiographs of the child – a standard that cannot be compromised. ‘If you miss minor fractures, you risk missing child abuse,’ Van Rijn warned. This thoroughness is justified by compelling statistics: one-third of children examined for a reported fracture have additional unreported fractures, and 40% of abusive head trauma cases reveal additional fractures elsewhere in the body.2
This meticulous approach to follow-up imaging ensures that no signs of healing trauma are missed, providing critical evidence for identifying abuse
Rick R. Van Rijn
The follow-up survey, conducted after two weeks, requires fewer images but remains essential. At the follow-up, radiographs should include the chest in three directions, upper and lower arms, upper and lower legs, and spot radiographs of areas with initial concerns or identified metaphyseal fractures.
Van Rijn illustrated the importance of this with a case of a 7-week-old with whooping cough whose follow-up radiographs revealed healing posterior rib fractures only visible after callus formation had begun – a clear indicator of previous trauma that would have otherwise gone undetected. ‘This meticulous approach to follow-up imaging ensures that no signs of healing trauma are missed, providing critical evidence for identifying abuse. However, imaging should not stop at skeletal surveys – neurological imaging plays an equally vital role in uncovering hidden patterns of abuse.’
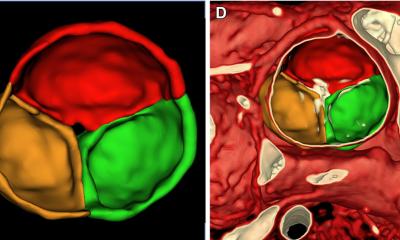
Advanced neurological imaging: beyond the obvious
Neurological imaging extends beyond cases with clear symptoms of abuse. ‘This isn't just for clinical findings but for forensic purposes,’ Van Rijn clarified. ‘There's a strong pattern of recurrent trauma in these cases.’
Neurological imaging is essential in two key scenarios: when a child presents with neurological symptoms, and even when no neurological symptoms are apparent but physical abuse is suspected. Van Rijn underscored the importance of imaging in the latter scenario by recounting a chilling example from a French study. ‘In some cases, caregivers admitted to shaking their child to make them fall asleep. It worked – until one day, the child didn’t wake up anymore. It died,’ he explained.
‘It's a strong hallmark – a known trauma that indicates the child has probably been abused,’ Van Rijn emphasized the importance of neurological imaging for forensic purposes. This evidence provides an entry point to engage with parents and offer support. ‘No one wakes up and says, “I will kill my child.” Abusers often come from poor backgrounds, suffer from psychological disorders, or have experienced abuse themselves in their youth.’
Protecting the siblings: extending the safety net
When abuse is identified, the investigation shouldn't stop with the index patient. According to the international consensus statement published in JAMA Pediatrics3, all contact children should be screened based on age-specific protocols:
If no findings indicative of abuse are observed, the child is screened as a contact child using age-based protocols:
- Under 1 year: Perform a brain MRI (adding spine MRI if brain findings are abnormal) and a full skeletal survey.
- Ages 1–2 years: Perform a full skeletal survey.
- Ages 2–5 years: No radiological screening is required unless physical findings suggest abuse.
If findings indicative of abuse are present, the child is investigated as per national guidelines for an index case.
A call to action
‘It only takes one radiologist to stop child abuse,’ Van Rijn concluded, noting that an international consensus guideline for imaging in suspected child physical abuse (IGISPA) is in development. His message was clear: radiologists armed with proper protocols and vigilance can make life-changing – and potentially life-saving – differences for vulnerable children.
References:
- Felitti VJ, Anda RF, Nordenberg D et al.: Relationship of childhood abuse and household dysfunction to many of the leading causes of death in adults. The Adverse Childhood Experiences (ACE) Study; American Journal of Preventive Medicine 1998; https://doi.org/10.1016/s0749-3797(98)00017-8
- Loos MLHJ, Ahmed T, Bakx R, van Rijn RR: Prevalence and distribution of occult fractures on skeletal surveys in children with suspected non-accidental trauma imaged or reviewed in a tertiary Dutch hospital; Pediatric Surgery International 2020; https://doi.org/10.1007/s00383-020-04706-z
- Mankad K, Sidpra J, Mirsky DM et al.: International consensus statement on the radiological screening of contact children in the context of suspected child physical abuse. JAMA Pediatrics 2023; https://doi.org/10.1001/jamapediatrics.2022.6184
02.07.2025