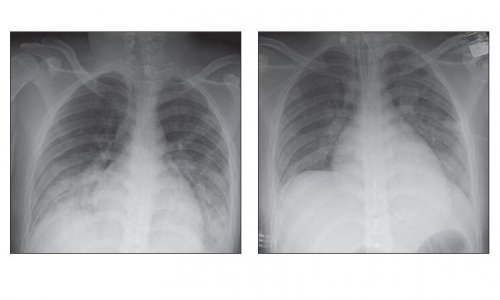
Image source: Adobe Stock/ Сергей Уланов
News • Joint statement from BIR and UKHSA
Radiation dose: clinical need should trump previous exposures, experts say
The UK Health Security Agency (UKHSA) and the British Institute of Radiology (BIR) issued a joint position statement that supports the view that the decision to perform a medical imaging exposure should be based on clinical need rather than the dose from previous exposures.
The position statement can be downloaded here.
In May 2021, the International Atomic Energy Agency (IAEA) published a joint position statement with a range of international organisations and professional bodies and call for action to strengthen radiation protection of patients undergoing recurrent radiological imaging procedures. The IAEA highlighted the potential for automatic exposure monitoring systems to monitor cumulative dose at an individual patient level. The joint position statement proposed actions to address concerns over high cumulative doses from recurrent medical imaging including, identification of clinical conditions that require recurrent imaging and developing strategies in terms of the type of imaging and frequency. It also recommended the need for customised imaging protocols for these patients and use of the latest technology to help reduce patient dose. Further actions include strengthening radiation protection education and training of healthcare professionals and strengthening communication.
To protect patients from unnecessary medical exposures, appropriate justification of medical imaging exposures is essential
UKHSA/BIR joint statement
Notably, the joint position statement recommended that dose monitoring systems should be used to monitor the exposure history of individual patients using type of radiological procedure, estimated effective dose or patient-specific organ dose estimates. The joint position statement recommended where possible, clinical and radiation dose information from the patient’s previous imaging procedures needs to be made available to help strengthen the decision-making process when justifying a series of radiological procedures for a patient.
In response to the joint position statement, the American Association of Physicists in Medicine (AAPM), the American College of Radiology (ACR), and the Health Physics Society (HPS) published a policy on the use of dose metric tracking for medical exposures. The AAPM consider that the decision to perform a medical imaging exam should be based on clinical grounds, including the information available from prior imaging results, and not on the dose from prior imaging-related radiation exposures.
The AAPM advise that justification of the potential patient benefit and optimisation of medical imaging exposures are the most appropriate actions to take to protect patients from unnecessary medical exposures. It further recommends against using dose values, including effective dose, from a patient’s prior imaging exams for the purposes of medical decision making, as the use of cumulative effective dose may have a negative impact on patient care.
UKHSA and BIR recognise the benefits of exposure monitoring systems in the optimisation process, while noting that there is no IEC standard governing the estimation of effective dose. Both organisations support the views outlined by the AAPM that the decision to perform a medical imaging exposure should be based on clinical need rather than the dose from previous exposures. In exceptional cases, when planning multiple high dose interventional (or CT perfusion) procedures exposing the same area, over a short time period, and where deterministic effects are expected, previous dose information should also be considered in the justification and optimisation process.
To protect patients from unnecessary medical exposures, appropriate justification of medical imaging exposures is essential. Optimisation of medical imaging exposures is one of the fundamental principles of the Ionising Radiation (Medical Exposure) Regulations and is required to keep doses from medical exposures as low as reasonably practicable, consistent with the intended purpose.
Source: UK Health Security Agency / British Institute of Radiology (OGL 3.0)
07.07.2023