Personalized therapy concepts maximize clinical benefit
For the 19th consecutive year the annual meeting of the European Society of Radiology (ESR), the European Congress of Radiology (ECR), takes place in Vienna.


From 7 to 11 March, more than 20,000 participants are gathering at the Austria Center Vienna to exchange medical imaging knowledge and to present the most recent research results. “MR/PET: a match made in heaven or hell?” It was Professor Heinz-Peter Schlemmer, Director of Radiology at the German Cancer Research Center in Heidelberg, who raised this question at the congress’ opening press conference. While some experts are outright euphoric in view of the possibility to acquire morphological as well as functional information in a single exam, Professor Schlemmer pointed out, others tend to be more skeptical about the combination of positron emission tomography (PET) and magnetic resonance imaging (MRI). The crucial issue, the radiologist added, is: “What is the medical benefit?”
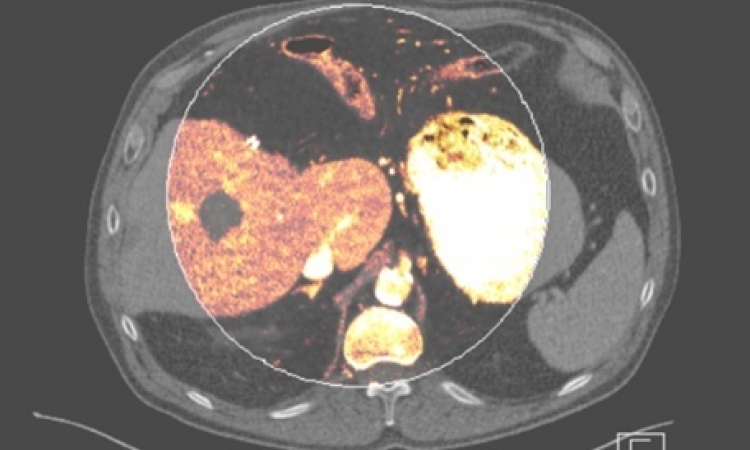
Many comparative studies have indicated that MRI and PET provide best results with regard to the detection of solid tumors. “Those results led us to believe that the combination of these two methods would yield the ideal procedure to detect and classify lesions”, Schlemmer said. Finally, in 2006, the first MR/PET scan was performed. Today, there are approximately 30 systems worldwide that can acquire such images. The technology allows the visualization of a tumor in high anatomical detail with MRI while PET offers information on metabolic processes and membrane receptors.Nevertheless, Schlemmer underlined, reining in the MR/PET euphoria, we have to gather more data. It is as yet unclear whether simultaneous imaging provides indeed higher accuracy than sequencing and how large the added value of MR/PET in comparison to the established PET-CT procedure really is. “A new technology, no matter how promising it may be, must never be integrated in daily clinical practice without scientific evidence and the evaluation and discussion of data regarding its diagnostic accuracy, impact on therapy management and economic efficiency,” the expert emphasized and added: “We have to prove it.”
A combination, however, which is successful beyond doubt is the intensifying cooperation between radiology and radiotherapy. “Diagnosis and therapy have long been separated – now it is high time for these two disciplines to join again,” Professor Regina Beets-Tan of the University of Maastricht in the Netherlands said.
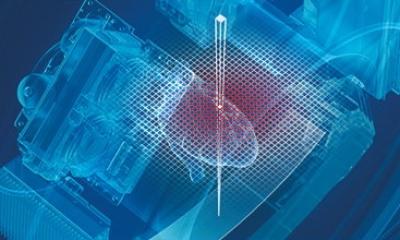
Due to technological progress and many innovative treatment approaches the cooperation of the two disciplines has led to highly efficient oncological therapies. Radiology uses functional imaging to gather information on metabolic processes in tumors. Thus particularly aggressive tumor areas can be identified and hidden metastases can be detected. Radiotherapists on the other hand use new technologies to target radiation and to control its intensity. Dose painting for example allows precise targeting of high dose radiation without impacting surrounding tissue as well as the application of different doses in different areas of the region of interest.
“These developments will enable us to pursue personalized therapy concepts which maximize the clinical benefit while reducing costs,” Professor Beets-Tan said. The European Society of Radiology (ESR) and the European Society for Radiotherapy and Oncology (ESTRO) have recognized the impact of such synergies and strongly promote cross-disciplinary training and education.
08.03.2013