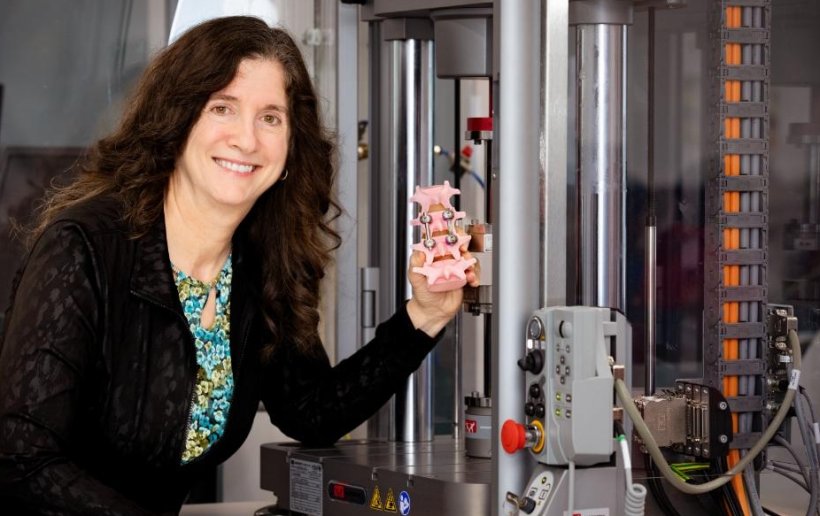
Image source: University of Canterbury
News • Device and software
New prototype to take the guess work out of spinal surgery
Spinal fusion is a highly invasive surgery where an implant is placed in the spine to prevent movement between bones. The treatment has a high failure rate after only five years. However, Associate Professor Debbie Munro, researcher and lecturer at the University of Canterbury (Te Whare Wānanga o Waitahi), has spent the last 20 years finding a way to change this.
Associate Professor Munro has developed a prototype device that attaches to a rod inserted during a spinal fusion surgery, akin to a strain gauge. Alongside this, she invented a wireless sensor and software to interpret outputs from the gauge, which will help determine the success of the fusion. “Currently surgeons cannot be certain the surgery has been successful before they suture a patient up, and they won’t know until around the four-month mark where you can see it on an x-ray. In New Zealand surgeons don’t x-ray the patient at all, if they aren’t in pain after 12 weeks they return to work,” Associate Professor Munro says.
The progress can feel very slow. Many patients undergoing this surgery are young or in skilled labour and find sticking to this treatment plan difficult, but with this device they could actually see their rate of improvement
Debbie Munro
“However, if the device has failed, they generally don’t know until three to four months post-surgery. At that point they begin the entire process again – requiring a second highly invasive surgery to replace the device. More bone is taken from the pelvis, crushed up and spread over the spine to stimulate bone growth which creates the fusion. When the sensor is first implanted it should display the maximum strain, if my software is showing there is no strain then the surgeon knows it hasn’t worked and can fix the problem before suturing the patient. Sometimes there are tiny cracks or a slightly loose screw within the implant, things invisible to the human eye, that may prevent fusion from working.”
Once the surgery has been found successful the device would be used to track the patient’s progress. “Spinal fusion surgery requires weeks of bedrest, and the progress can feel very slow. Many patients undergoing this surgery are young or in skilled labour and find sticking to this treatment plan difficult, but with this device they could actually see their rate of improvement.”
Currently there is a disconnect between those who need the surgery and where the surgeons are, and the multiple checks-up required can be another barrier for patients. “This device would allow a self-service style of care... the patient could scan the site themselves and the data would be sent to the surgeon, and the patient would only need to see the surgeon face-to-face if there was an issue.”
The device and accompanying software have long-term benefits for the patient too, “Not only can the device remain in the person forever as there are no batteries, so no risk of leakage, but if someone with this implant was in an accident, they could easily check whether the fusion had been impacted.” Associate Professor Munro also believes this technology could be used in other parts of the body, such as hip and knee replacements to track degradation. Further testing will occur over the next year with hopes it will be ready for commercial interest in early 2024.
Source: University of Canterbury
05.09.2023