image source: Adobe Stock/PIC4U
News • Focus on protein GDF15
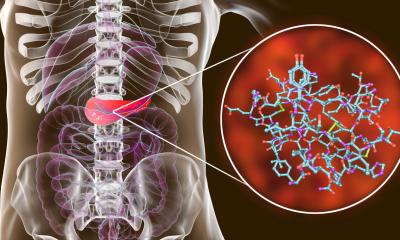
Newfound mechanism could improve efficiency of diabetes treatments
A study led by the University of Barcelona and the Biomedical Research Networking Center in Diabetes and Associated Metabolic Disorders (CIBERDEM) reveals how a new mechanism could improve the efficiency of currently available treatments for diabetes.
The study, carried out on mice and cell cultures, may open up new ways of approaching metabolic diseases that are a global health problem. The study, published in the journal Metabolism, focuses on the GDF15 protein, a factor that is expressed at high levels in many diseases, such as heart failure, cancer and fatty liver disease. Obese patients also have elevated levels of this protein, but its function is altered and those affected may develop resistance to GDF15 — that is, a reduction in the effectiveness of its activity.
The study is led by Professor Manuel Vázquez-Carrera, from the Faculty of Pharmacy and Food Sciences of the UB, the Institute of Biomedicine of the UB (IBUB), the Sant Joan de Déu Research Institute (IRSJD) and CIBERDEM. The study also highlights the participation of researchers Patricia Rada and Ángela María Valverde, also collaborators at CIBERDEM, the Spanish National Research Council (CSIC) and the Autonomous University of Madrid (UAM). The work has the collaboration of Professor Walter Wahli of the University of Lausanne (Switzerland), among other experts. "Our study reveals that GDF15 inhibits glucose synthesis in the liver. This pathway plays a decisive role in the generation of hyperglycaemia (increased blood glucose levels) in patients with type 2 diabetes mellitus", says Professor Manuel Vázquez-Carrera. "The action of the protein would also help reduce the presence of liver fibrosis, a condition associated with increased mortality in patients with fatty liver disease."
These results suggest that modulation of GDF15 levels could be useful to improve the effectiveness of current anti-diabetic treatments
Manuel Vázquez-Carrera
The study reveals that mice deficient in GDF15 have glucose intolerance and low levels of AMPK protein in the liver, which is a sensor of energy metabolism in the cell against type 2 diabetes. Moreover, increased glucose synthesis in the liver (hepatic gluconeogenesis) was also detected in these study models, as well as increased liver fibrosis.
All indications are that all the described alterations were triggered by increased hepatic levels of transforming growth factor-beta 1 (TGF-β1) and an SMAD3mediator protein, which are the main inducers of liver fibrosis. Thus, treatment with recombinant CDF15 can activate AMPK and decrease levels of active SMAD3 in mouse liver and in primary hepatocyte cultures.
"In conclusion, the results indicate that GDF15 activates AMPK protein and inhibits hepatic gluconeogenesis and fibrosis through the reduction of the TGF-β1/SMAD3 pathway", says Vázquez-Carrera. "These results suggest that modulation of GDF15 levels could be useful to improve the effectiveness of current anti-diabetic treatments, as hepatic gluconeogenesis is key in hyperglycaemia in patients with type 2 diabetes mellitus, and serum TGF-β1 levels are also increased in these patients", concludes the researcher.
Source: University of Barcelona
13.02.2024