New concepts for dose reduction in the diagnosis of coronary heart disease with CT
By Prof Stefan Schönberg of IKRN
Professor Stefan Schönberg of the Institute of Clinical Radiology and Nuclear Medicine (IKRN), University Hospital Mannheim, Medical Faculty of Mannheim, University of Heidelberg, invited colleagues from Mannheim and the Federal Office for Radiation Protection (BFS) in Neuherberg for a round-table discussion on: Non-invasive multidetector coronary CT angiography (CTA) has become an established imaging tool for the diagnosis of coronary artery disease.
Several studies have shown that – particularly with new scanner generations (i.e. 64-slice and higher) – the presence of hemodynamically relevant coronary artery stenoses in previously untreated patients can be ruled out by CT with a high negative predictive value of almost 100%. With the latest 4th generation CT systems, which use broader detector arrays with up to 320 rows or dual source technology, an isotropic spatial resolution of 0.5 mm and a minimal temporal resolution of 83 ms can be realised, which approaches the spatial resolution of catheter-based coronary angiography (~0.3 mm).
However, with CT the patient is exposed to considerably higher amounts of ionising radiation than with standard catheter-based coronary angiography. In recent clinical CTA studies using a 64-slice scanner, the effective dose ranged between 10 and 21 mSv, in comparison to 5 to 6 mSv for a diagnostic catheter-based coronary angiography. Recent radio-epidemiological estimates have shown that standard cardiac scans are associated with a considerable risk for patients to develop a radiation-induced cancer. As expected, the so-called lifetime attributable risk (LAR) for cancer incidence depends markedly on the age at exposure and the gender of the patient: It is markedly higher for women and younger patients as compared to men and older patients (LAR for standard cardiac scans varied from 1 in 143 for a 20-year-old woman to 1 in 3261 for an 80-year-old man).
To maintain low levels of image noise and thus high image quality in CTA, the current-time product and tube potential must be increased with increasing patient body size or decreasing slice thickness.
Several techniques have been developed to the reduce radiation exposure related to a CT examination of the coronary arteries. The radiation dose decreases considerably by applying a lower tube potential. Recent studies have shown that reducing the tube potential in CTA from 120 kV to 100 kV in patients of normal weight results not only in a marked reduction of the radiation dose but also improves the contrast between vessels filled with an iodinated contrast agent and their surroundings. One of the most promising techniques to reduce patient exposure in MSCT is that of automatic tube-current modulation, which allows substantial radiation dose reduction without sacrificing image quality. The principal idea of this approach is to adapt the tube current according to the changing anatomy of the patient, both, in the transverse as well as axial direction. Coronary arteries typically show the least motion in the diastole. Therefore, images required to diagnose patients with low heart rates should be reconstructed from diastolic data. By contrast, systolic data does not necessarily need to be reconstructed. This can be realised by the ‘ECG-controlled tube-current modulation’, which decreases or switches off X-ray tube current during systole.
Quantification of the calcium content in coronary arteries by electron beam CT and MDCT was traditionally used with prospective ECG triggering with sequential slice-by-slice acquisition, and is typically related with a radiation exposure of about 2 mSv. To achieve a high reproducibility of coronary CTA, it is essential to use short acquisition times and overlapping slice reconstruction (to reduce partial-volume effects). With previous MDCT scanner generations this could only be realised by retrospectively ECG triggered helical acquisition of the coronary artery tree. With the current MDCT technology, however, much shorter acquisition times can be realised, which makes prospective ECG triggering possible. By using the so-called ‘step and shoot (SAS)’ mode, the X-ray tube is turned on only during predefined phases of the cardiac cycle, while the table is moved in the remaining phases not utilised for data acquisition. This approach considerably reduced radiation exposure of patients. When the axial range covered by the detector rows in MDCT is increased, the dataset can be acquired within only few heartbeats (or only one with most recent technology), which can result in dose reduction.
Most of these technological approaches can be combined to optimise CT examinations of the coronary arteries from a radiation hygienic viewpoint. Initial studies revealed that the effective dose can be reduced to less than 5 mSv, which is comparable or lower than the dose related to diagnostic X-ray coronary angiography.
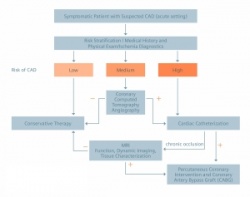
Nevertheless, restricting the indication to a well-defined patient population is still the best method for reducing radiation dose of patients. In patients with a high pre-test probability of coronary stenoses there is a high likelihood that interventional treatment will be necessary anyway and there would be no clinical benefit of CTA. Considering the radiation dose, there is also no evidence for screening of low risk patients or asymptomatic individuals. The benefit of CTA is likely to be greatest and is reasonable for symptomatic patients who are at intermediate risk for coronary artery disease (CAD) after initial risk stratification, including patients with equivocal stress-test results. In consideration of recent scientific statements and study results, a clinical algorithm for the diagnosis of CAD with the use of CT was established at our institution (Figure 1). A symptomatic patient with suspected CAD has to undergo a risk stratification including physical exam, ischemia diagnostics and medical history first. CTA is a central tool for patients with a medium risk value (10–90%).
With its high negative predictive value one can be confident to adhere to conservative therapy after negative CTA (no or low grade stenosis only). Even in these patients, findings such as extended noncalcified or calcified coronary plaques warrant intensification of conservative therapy, so there is an additional benefit for the patients. Patients with positive findings (high grade stenosis) are referred to cardiac catheterisation with potential percutaneous coronary artery intervention. The pre-interventional CT also helps to plan the procedure and is a valuable means of image-guided therapy. Patients with chronic coronary artery occlusion confirmed at catheter angiography are referred to MRI for the assessment of viability, in order to evaluate if the patient benefits from a revascularisation procedure.
The algorithm is currently evaluated as part of a research project performed in collaboration with the Federal Office for Radiation Protection in Germany. To its end, a comprehensive benefit-risk evaluation of various non-invasive imaging tools available for the diagnosis of CAD (MDCT, MRI, PET/CT, coronary angiography) will be performed, taking into account risks from the imaging technique, the administration of contrast agents, and the invasiveness of the procedure.
06.11.2008