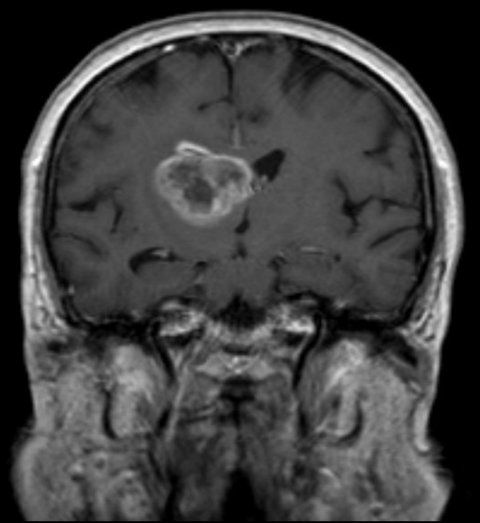
News • Glioblastoma
New actively personalized therapeutic vaccine for brain cancer
The prospect of an actively personalized approach to the treatment of glioblastoma has moved a step closer with the recent publication in Nature* of favorable data from the phase 1 study GAPVAC-101, testing a novel therapeutic concept tailored to specific characteristics of patients’ individual tumors and immune systems.
For the first time, the feasibility of such a highly personalized form of immunotherapy has been exemplified in a multi-center, multi-national clinical setting. Glioblastoma, an aggressive form of brain tumor with poor prognosis, has a high unmet need and the limited treatments available today have minimal effect on overall survival. To date, patients with glioblastoma have not sufficiently benefited from recent breakthroughs with checkpoint inhibitors – to a great part, because this tumor type is characterized by a low mutational load and thus only few neoantigens are targetable by the immune system.
The Glioma Actively Personalized Vaccine Consortium (GAPVAC) approach is a highly personalized method being progressed through the GAPVAC-101 first-in-human clinical trial by a European Union-funded consortium, led by Immatics Biotechnologies GmbH (Tuebingen, Germany) and BioNTech AG (Mainz, Germany).
Fifteen newly diagnosed glioblastoma patients received two therapeutic vaccines in succession; the first being actively personalized vaccine 1 (APVAC1) targeted at non-mutated antigens, followed by APVAC2 preferentially targeted at neo-antigens. Vaccine compositions were personalized for each patient based on analysis of the transcriptome, immunopeptidome and mutanome of the individuals’ tumors and, for APVAC1, also based on the capability of each patient to mount an immune response. Both vaccine types displayed favorable safety and immunogenicity. Non-mutated APVAC1 antigens induced sustained central memory CD8+ T-cell responses, whilst APVAC2 induced T helper cell type 1 (TH1) CD4+ as well as CD8+ T-cell responses against predicted neo-epitopes.
Patients in this study were treated at six European centers: The University Hospital of Heidelberg (Germany), the University Hospital of Tübingen (Germany), the Geneva University Hospital (Switzerland), the Leiden University Medical Center (The Netherlands), the Rigshospitalet (Copenhagen, Denmark), and the Vall d’Hebron University Hospital (Barcelona, Spain). Furthermore, the Department of Immunology, University of Tübingen (led by Prof. Hans-Georg Rammensee), BCN Peptides (Barcelona, Spain), the Association of Cancer Immunotherapy (CIMT), the University of California San Francisco (US), the University Southampton (UK), and the Technion-Israel Institute of Technology (Haifa, Israel) participated in the study involving a pioneering concept, complex manufacturing, logistics and various biomarker analyses.
Recommended article
News • Tumor research
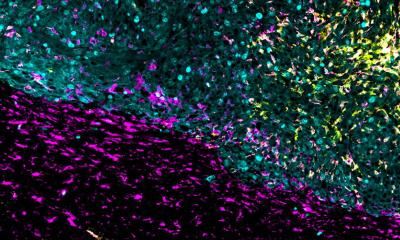
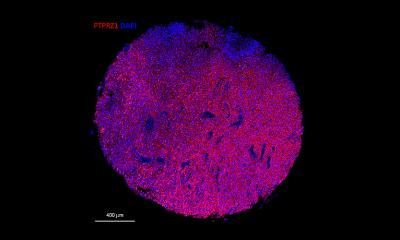
Growing brain cancer in a dish
Austrian researchers have accomplished an astounding feat: They created organoids that mimic the onset of brain cancer. This method not only sheds light on the complex biology of human brain tumors but could also pave the way for new medical applications.
The insights gained will contribute to future immunotherapy efforts to bridge the precision of genomic medicine and immunotherapy for the benefit of patients
Wolfgang Wick
The trial was led by the Principal Investigator (PI) Prof. Dr. Wolfgang Wick, University of Heidelberg and German Cancer Consortium (DKTK). Prof. Dr. Pierre-Yves Dietrich, University of Geneva, also an internationally recognized expert in the treatment and immunology of brain cancer, served as Co-PI. “The ability to exploit the full repertoire of tumor antigens, including non-mutated and neo-antigens, may offer more effective immunotherapies, especially for tumors with low mutational load”, said Prof. Dr. Wolfgang Wick, Chair of the Neurology Clinic at the Heidelberg University Hospital. He added: “The trial approach combines exceptional science and a rigorous protocol for a disease for which over-simplified strategies have failed in the past. In addition, the insights gained will contribute to future immunotherapy efforts to bridge the precision of genomic medicine and immunotherapy for the benefit of patients. We believe that it provides a blueprint for future trials in personalized medicine.”
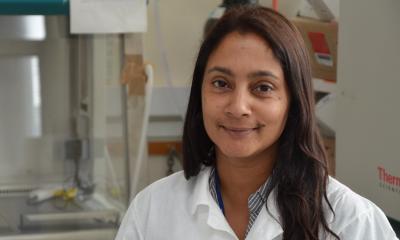
Dr. Harpreet Singh, Chief Scientific Officer of Immatics Biotechnologies GmbH and Coordinator of the GAPVAC consortium, said: “We are at a very exciting stage in the evolution of personalized cancer treatments, building on the scientific advances in immuno-oncology and checkpoint inhibitors. The protocol used in GAPVAC-101 is an entirely new, personalized approach to treating cancer that combines the innovative science of all of the consortium members. We are excited that we have been able to achieve such a high degree of treatment personalization due to our ability to perform mass spectrometry, next generation sequencing, mRNA microarray, immune repertoire analysis and drug manufacturing for every patient.”
Prof. Dr. Ugur Sahin, Chief Executive Officer of BioNTech AG and Vice Coordinator of the GAPVAC consortium, noted: “The GAPVAC consortium is one of the first groups in the world that aim to target mutations in glioblastoma to optimize drugs for each individual patient. The high immunogenicity rate of vaccine targets detected in this collaborative study indicates that even tumors with low mutational load such as glioblastomas are amenable for individualized immunotherapy approaches.”
Source: Heidelberg University Hospital and Medical Faculty
20.12.2018