Article • Hirnübungen I
Neuro MR: What‘s new in brain tumors?
From the extremely new, but not very available, to the somewhat new, very available and highly useful, Walter Kucharczyk will cover the potentials and practicalities in advanced brain tumor imaging.
When the organizers of Garmisch MR 2017 wanted to hear about the newest developments in neuro radiology, they turned to Walter Kucharczyk, MD, FRCPC, one of the event's most experienced presenters, having delivered lectures at this MRI Symposium since 1991. His experience also includes having served as the president of the International Society of Magnetic Resonance in Medicine (ISMRM), the largest research and education group in the world devoted to developing and teaching magnetic resonance to doctors and scientists, and as previous Professor and Chair of the Department of Medical Imaging at the University of Toronto for 16 years. He is a veteran lecturer with a decades-long record of international lectures.
The faculty's proposed title for the talk was terse, yet ambitious:
“Brain tumors: what is new?”
Among the delegates attending his presentation, Prof. Kucharczyk said that while many will be interested in and aware of the very newest developments in neuroradiology, most practitioners will be not have access to such equipment and methods, so they will looking for advanced, “somewhat-new” techniques that may not be the newest, but are available, are of proven value, and have stood the test of time.
“For this reason, I will be dividing the lecture into two between readily available, useful methods, that may not be extremely new, and what is truly new, but not readily available, is complicated to analyze, and thus not particularly useful to most radiologists in the clinic today?“, he said. “I hope both parts of the lecture will be of interest to the audience – letting them know what all of them can do today and giving them a taste of what might be useful in the near future.
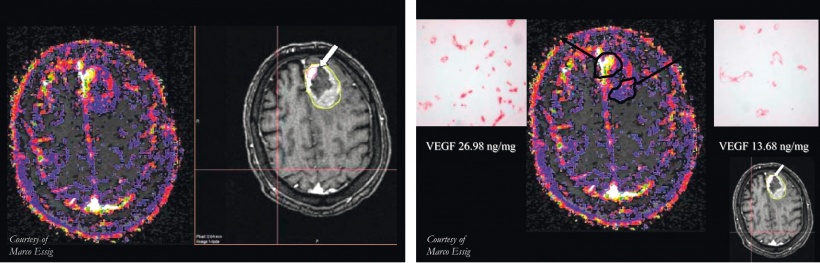
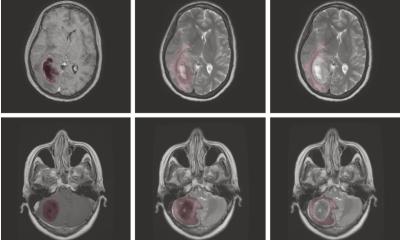
images credit of Prof. Dr. Marco Essig, Department of Radiology, WRHA, Canada
After setting a context in reviewing the not-so-new, but well-proven techniques, Prof. Kucharczyk will advance into more recent developments in techniques that he said are sufficiently available that everyone can use them, and which are useful for a variety of applications, including diffusion weighted imaging, tractography, perfusion MRI, and MR spectroscopy.
The very newest techniques are mostly done in the research environment to investigate and help solve yet unsolved problems. But they are not widely practiced because not every medical imaging center has the hardware, software, cyclotron, combined MRI-PET scanner, carbon hyper-polarizer, or specialized personnel to perform these techniques. “I don’t think we are there yet with many of the very newest things“, he said.
I don’t think we are there yet with many of the very newest things.
Prof. Walter Kucharczyk
The usefulness of the most readily radio-tracer, 18-FDG, for imaging brain tumors is limited, he said, because radiotracers based on glucose provide poor image contrast between the tumor and normal brain. Brain tumors and healthy brain tissue both avidly take up the glucose.
“As a result you need to go to other novel formulations of radiotracers, which are very expensive and have very short half lives“, said Prof Kucharczyk. “These necessitate having a cyclotron”.
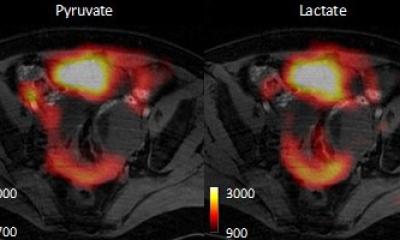
“Similarly hyper-polarized carbon species carry similar logistic and cost issues of requiring a very expensive carbon hyper-polarizer, but do enable the radiologist to study carbon-based metabolites such as pyruvate through its biochemical pathways and potentially assess the effectiveness of therapeutic drugs. But very few people in the world have a carbon hyper-polarizer as it costs something north of a million dollars, and then it has to be placed beside the scanner as the tracers have very short half-life”, he said.
The lecture would not be complete without a discussion of developments that Prof. Kucharczyk said falls into the category of automated image analysis, big data and machine learning.
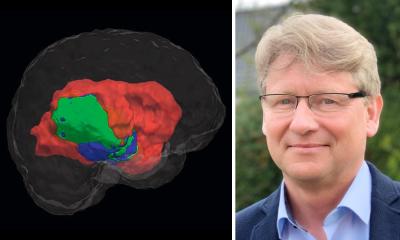
“There is work being done on very interesting concepts based on automated image analysis and machine learning. When we humans look at an image we see patterns that are based on the spatial location of dots, their gray scale or color, and shapes. But digital images can yield additional information already embedded in them, based spatial frequencies and similar features, that can only be extracted by various mathematical operations and transforms, and not appreciated by the human eye”, he said.
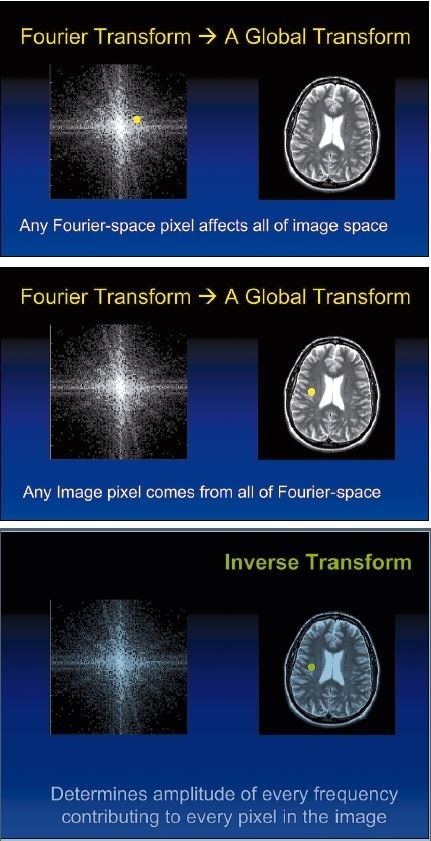
“When we analyze this scatter image we can‘t say if it is a picture of a human brain or a giraffe. But with appropriate software a computer can recognize patterns that we cannot, potentially finding unique patterns that may ultimately prove diagnostic of certain diseases. By analyzing sufficiently large sets of such image data, perhaps soon automated analysis will enable us to distinguish between various types of brain tumors, grade them, and possibly even inform us of their genetic makeup”, he said.
Wouldn't it be cool if we could actually determine the same findings from the images as the pathologist does from the microscopy?
Prof. Walter Kucharczyk
Looking ahead, Prof. Kucharczyk said he hopes that radiologists, like machines, can learn from the detailed correlative analysis of clinical information, images, and pathology studies to deliver findings that increasingly correlate with the ultimate pathology report.
“As radiologists, we are quite accurate in macroscopic diagnosis. We can see many things about a brain tumor that pathologist does not: the extent of a tumor, its size, and whether there is more than one tumor. And we can provide a fair estimate of the grade and histopathology of the tumor.
Today the pathologist has the final say in brain tumor diagnosis, and by definition has the definitive opinion on grade, mitotic rate, histopathology, and genetic profile, with terms such as: 1p19q co-deletion to determine the chromosomal type, IDH 1 and 2 mutation (isocitrate dehydrogenase), and the MGMT promoter methylation status. These are all important in determining diagnosis, prognosis, and probability of treatment response“, he explained.
“Wouldn't it be cool if we could actually determine the same findings from the images as the pathologist does from the microscopy?”, he asks.
“Ultimately our objective should be to be able to do everything the pathologist does, but to do it in vivo, by extracting that information from images. Our objectives should be to determine all features of the diagnosis and prognosis without having to operate on the patient, without having to extract tissue. Are we there yet? No way. Will we ever get there? Probably not completely, but we are moving in that direction“, said Prof. Kucharczyk.

Profile:
Walter Kucharczyk, MD, FRCPC is the Director for Research at the Joint Department of Medical Imaging of the University of Toronto and a hands-on Neuroradiologist there, as well as a Professor of Medical Imaging and Neurosurgery. He is an author for 140 peer-reviewed publications in the field, holds numerous peer-review and industry sponsored research grants, and is a co-holder of a patent on a MRI-compatible robot for minimally invasive procedures. No stranger to Germany, he did a one-year sabbatical in the department of mechanical engineering in the Institute of Advance Studies at the Technical University of Munich, focussing on image-navigation and robotics for medical procedures.
Veranstaltungshinweis
Samstag, 04.02.2017, 09:10-09:40 Uhr
Hirntumoren: Was gibt es Neues?
W. Kucharczyk, CAN-Toronto
Session: MRT des ZNS
04.02.2017