MRI scans help to define chemotherapy's effect
Faster assay for targeted chemotherapy's success against deadly liver cancer saves lives, and could speed lifesaving switch to alternative drug therapies for well-known pancreatic cancer.

Studies on some 55 U.S. men and women with potentially deadly liver or pancreatic cancers show that specialized MRI scans can tell within a month whether highly toxic chemotherapy is working and killing tumor cells long before tumors actually shrink – or fail to shrink.
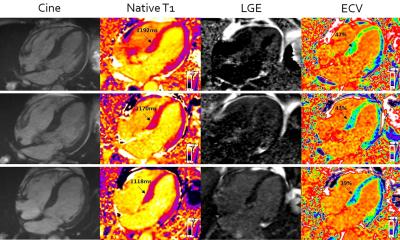
Using special software and MRI scanners, imaging experts at Johns Hopkins developed their new assay, known as a volumetric functional MRI scan, by exploiting the physiological differences in water movement and absorption inside cancer cells that are dying and those that are not.
The studies are believed to be the first to show that the diagnostic imaging procedure buys patients many months to well over a year of life, by figuring out who might benefit from repeat or higher-dose chemotherapy,
The paired scans, which take only minutes to perform, can detect the movement of water molecules inside tumor cells; and software performs the mathematical analysis needed to calculate the imaged tumor cells’ so-called apparent diffusion coefficient. Living tumor cells showing a low coefficient, as water absorption in and out of the cells is tightly controlled, and dying cells – the goal of chemotherapy – have a relatively high coefficient, because the tumor cells’ membranes have lost the ability to restrict water movement. The software used in the scans was developed at Johns Hopkins and at Siemens Healthcare Diagnostics, which manufactures the scanners.
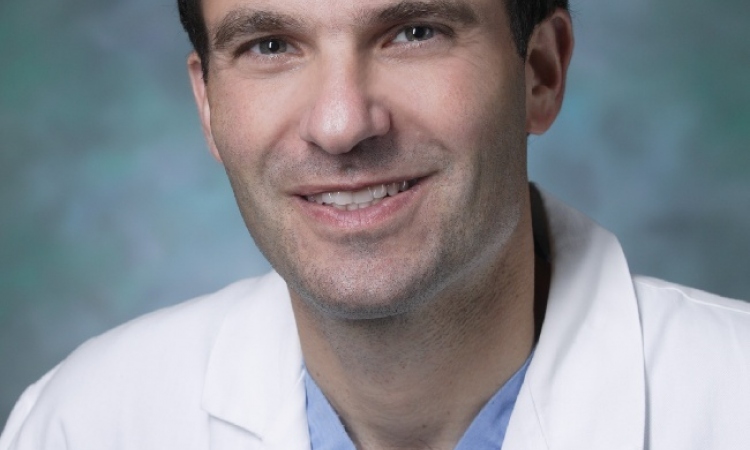
“Our latest volumetric functional MRI scans could help people with aggressive cancers, and little time to spare on failed treatments, know as quickly as possible if their treatment is working and when they need to consider other treatment options. And without having to wait for months to actually see tumor shrinkage,” says study senior investigator and radiologist Ihab Kamel, M.D., Ph.D.
Results from the first of two studies to be published in the same July 1 issue of the journal Radiology show that the high-precision, 3-D images, taken shortly before and one month after a form of chemotherapy called transcatheter arterial chemoembolization, could assess the treatment’s impact against a rare and advanced form of liver bile duct cancer, known as cholangiocarcinoma. The study involved 29 men and women aged 29 to 82, all undergoing treatment at The Johns Hopkins Hospital.
Among the key findings in the first study was that 22 people, whose functional MRI scans showed increases in apparent diffusion coefficient scores of over 45 percent, lived at least 10 months longer, while some 17 with coefficient score increases over 60 percent, lived at least 17 months longer.
Kamel, an associate professor at the Johns Hopkins University School of Medicine and its Russell H. Morgan Department of Radiology, says that cholangiocarcinoma is often diagnosed at such an advanced stage that patients only have on average six months to live. “By the time our patients become jaundiced, start turning yellow from bile buildup and seek medical help, it’s almost too late,” he says. “They have no time to waste on failed treatments.”
The second study, also at Johns Hopkins, tested the scans on 26 men and women, ages 37 to 79, with islet cell carcinoma, a well-known pancreatic cancer. Researchers analyzed some 215 tumorous lesions in these people, scanning shortly before and one month after the same initial treatment for their cancer.
Kamel says physicians have more treatment options with islet cell carcinoma and can switch people from chemoembolization to chemotherapy with either drug Sunitinib or Everolimus.
Results in the second study showed that for 78 tumors, which responded well to chemotherapy, functional MRI scans produced apparent diffusion coefficient score increases averaging at least 70 percent, while in the 137 tumors for which treatment was not a success, increases in coefficient measures averaged less than 40 percent. Treatment was considered successful if tumor shrinkage continued for at least six months.
“Our analysis shows how to clearly define and demarcate between patients whose tumors are responding to treatment and those who are not,” says Kamel. This is very important, he adds, because in islet cell carcinoma, some patients’ cancer symptoms, such as headaches, ulcers, pain and diarrhea, can be masked by the liver’s hormone production. The disappearance or absence of symptoms is not a reliable indicator of treatment success.
Larger studies already planned will measure how well the apparent diffusion coefficients for each kind of combination chemotherapy predict survival and how much time remains to switch treatment plans.
In transcatheter arterial chemoembolization, interventional radiologists thread an ultrathin catheter through an abdominal artery directly to the main arteries feeding the liver tumor. Drug-eluting beads are delivered to and released directly inside the tumor to kill it by cutting off its blood supply. The roughly half-hour procedure carries a slight risk of bleeding or damage to the blood vessels, while the toxic drug treatment can permanently damage otherwise healthy liver tissue. Most patients are discharged from the hospital within a day, and many are able to resume physical activity and work.
The Cholangiocarcinoma Foundation estimates that some 2,500 people are newly diagnosed each year with the bile duct cancer, most in the moderate to advanced stages of disease.
Studies have estimated that islet cell carcinomas account for at least 1.3 percent of the 44,000 new cases of pancreatic cancer in the United States each year.
Funding support for both studies was provided by Siemens Healthcare, of Princeton, N.J., the manufacturer of the MRI scanners used in the study.
08.06.2012