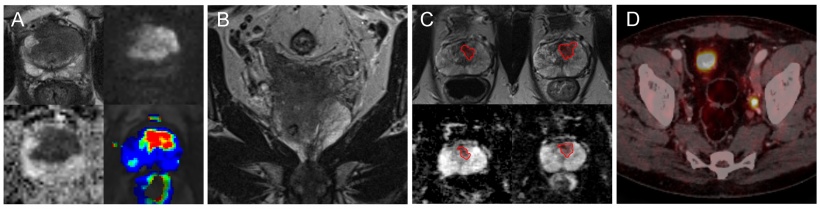
B: Staging: Extensive seminal vesicle invasion and lymph node metastases on a coronal T2-weighted turbo spin echo (TSE) MR-image
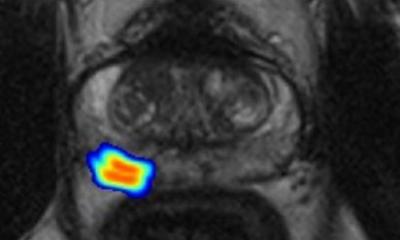
C: Active Surveillance: Tumour increase in size and aggressiveness (ADC-value decrease) in follow-up MRI in a patient with bioptic verified low-grad prostate cancer
D: Recurrence: PSMA-PET/CT with parailiac lymph node metastasis on the left side
Article • Recognition in new recommendations
MRI’s role in prostate cancer diagnosis
Lars Schimmöller MD, associate professor of radiology at Düsseldorf University Hospital, tackled current diagnosis of prostate cancer (PCa) and addressed tumour detection, staging, active surveillance and recurrence during the Medica Academy session on Imaging Update. He also highlighted how MRI helps improve biopsies and avoid unnecessary surgery in PCa.
Report: Mélisande Rouger
Asked about the latest advances in PCa diagnosis, Professor Lars Schimmöller spoke of ‘a remarkable change’ – the increasing role of magnetic resonance imaging (MRI) in routine clinical diagnosis. ‘In its updated guidelines, which will be published later this year, the German Society of Radiology notably insists on the importance of multiparametric MRI (mp-MRI) and MRI-guided biopsy for PCa diagnosis.
‘The new recommended technical approach is that mp-MRI can not only be used but also should be used in secondary PCa detection after negative transrectal ultrasound (TRUS)-guided biopsy and before inclusion of patients for active surveillance, similar to international guidelines. Moreover, the German preliminary recommendations for 2017 state that mp-MRI can be used for primary PCa detection as long as quality standards are fulfilled. Based on these requirements, urologists can and should perform targeted biopsies of MRI suspicious lesions, by using either the cognitive approach (fusion of MRI and US in mind) with TRUS or software-based MRI-US fusion-guided biopsy approach.

‘Five to ten years ago, the standard was to just measure prostate-specific antigen (PSA) value, carry out digital rectal examination, and then an ultrasound and US-guided systematic biopsy. The problem with systematic biopsy is that especially the anterior and apical parts of the prostate are not covered, and cancers missed or only partially captured with up to 50% false positive lower grade histology, so that you never know if higher-grade proportions of the tumour exist.
‘One of the big challenges in PCa is its biology. When you have multifocal tumour cells, which are quite common, it’s hard to get the real imaging of where the index lesion is located. Performing an MRI-guided biopsy and an mp-MRI examination before biopsy to help prepare it enables it to hit a tumour with more precision. If you have quality mp-MRI, you can say with over 95% accuracy if there is clinical relevant cancer or not.
‘Also, if you carry out an MRI examination before you do a biopsy, you may discover the reason for high PSA value. Sometimes it may just be prostate enlargement or an infection. So carrying out an MRI scan may also avoid performing unnecessary biopsies. Another significant advance in PCa diagnostics has been the use of prostate specific membrane antigen (PSMA) as a relatively new tracer to check PCa recurrence.’
Which diagnostic and imaging modalities do you use in PCa?
‘The PSA determination is the basic diagnostic tool for PCa check-up, but PSA is specific to the prostate gland and not prostate cancer. An elevation of PSA does not have to be associated with PCa, but when you use it wisely, it is an easy and excellent test for a preselection. The role of PSA screening has been extensively discussed, especially in over diagnosis and over treatment, but trial results from large European studies have shown the relevance of this test. We are currently trying to figure out when it makes sense and in whom – in patients aged 40, 45, 50 or 55 years?
‘Ultrasound is the standard urologic imaging modality, but US has limitations in PCa detection. It is not so good for sensitivity or specificity, even combined with contrast agents. Currently none of these additional US-tools are recommended for primary PCa detection. US is primarily used to guide biopsy.
Mp-MRI is currently the best imaging tool for prostate cancer detection, especially clinical relevant PCa.
Lars Schimmöller
‘Computed tomography (CT) only makes sense in combination with PSMA-PET, e.g. for PCa recurrence, or it may be chosen for pre-operative staging. CT is easily available and gives you an idea of metastases of bone lesion or lymph node metastasis in patients with extensive disease. But lymph nodes imaging is challenging, because they are often very small. CT is mostly not good at differentiating whether they are tumours or not in the prostate setting.
‘Mp-MRI is currently the best imaging tool for prostate cancer detection, especially clinical relevant PCa. Qualitative mp-MRI is extremely promising for active surveillance and furthermore it is good for local staging. It can also help in unclear cases or PCa recurrence.
‘PSMA-PET is the most promising imaging tool for PCa-recurrence and may be used for detection in unclear cases with high PCa suspicion. Combination of PSMA-PET with MRI might be very nice, but PET/MRI is rarely available and its clinical benefit remains to be demonstrated.’
Screening programs in Germany
‘The updated recommendation is that men of at least 45 years of age and a life expectancy of more than 10 years should be informed on the possible benefits and drawbacks of early-detection measures of prostate cancer like PSA determination.
‘We are performing a huge national prospective multicentre randomised trial on early PSA screening in young men. Currently we have over 30,000 patients enrolled. The study is called PROBASE and we try to assess if it makes sense to measure baseline PSA for risk-adapting PSA screening. Screening must help lower mortality. It only makes sense if you help people not to die or die later from that cancer. ‘PCa is most often a slow growing tumour, so that’s why screening studies results need so long to show their value. You need at least 10 to 15 years approximately to show if a patient benefits from screening.’
What are PCa imaging risks?
Mortality in PCa is often due to late cancer detection or inaccurate diagnosis.
Lars Schimmöller
‘Nationwide coverage of qualitative mp-MRI examinations and qualitative standardised reporting are two of the most important challenges in PCa imaging. Furthermore, the subsequent correct targeted biopsy is also a challenge for urologists and radiologists.
‘A further issue is that the biology of prostate tumours is often multifocal and/or heterogeneous in histology, and sometimes hard to differentiate from inflammation or atypical stromal hyperplasia. It is also complex to determinate the possible metastatic clone with current technology. It’s crucial to differentiate tumours that are life limiting from those who are not.
‘Mortality in PCa is often due to late cancer detection or inaccurate diagnosis. But most tumours are not life limiting or can be treated. Radiation risk, as a general limitation or challenge in radiology, is not a problem, because these patients are usually not young and MRI, as the best imaging tool, does not use radiation.’
Profile
Lars Schimmöller MD is Associate Professor of radiology and head of the uroradiology working group at Düsseldorf University Hospital, Germany. His research fields include multiparametric magnetic resonance Imaging (MRI) of the prostate, image-guided prostate biopsy, hybrid imaging (e.g. PSMA-PET), urogenital radiology and cancer imaging.
18.12.2017