Article • Benign breast diseases (BBD) and cancer incidence
More personalised breast screening needed
Women with incident and proliferative benign breast diseases (BBD) are likelier to develop breast cancer, a Spanish researcher explained during the 12th European Breast Cancer Conference in October. These findings support the idea of designing personalised breast cancer screening strategies to improve effectiveness.
Report: Mélisande Rouger

BBD, a group of non-cancerous breast disorders, have been proved to increase chances of subsequent breast cancer. New evidence has emerged that the time they are detected in a national screening programme indicates which lesions are likelier to become cancerous, according to a team at the Hospital del Mar Medical Research Institute in Barcelona.
‘Our results show that women with a benign breast disease diagnosed from the second screening onwards have a significantly higher subsequent risk of breast cancer than those with a BBD diagnosed on their first mammographic screening,’ said Dr Marta Román, a senior researcher in the epidemiology department at the Hospital del Mar Medical Research Institute, during the conference.
Proliferative BBD detected from 2nd screening onward linked with higher risk
BBD may be detected on the first occasion a woman attends breast screening, usually at age 50 in Spain, and are then classified as ‘prevalent’ BBD. Those BBD detected on subsequent visits, which occur every two years, are classified as ‘incident’ BBDs. With their study, just published in The Breast (Differences in breast cancer risk after benign breast disease by type of screening diagnosis), Román and her colleagues assessed differences in the risk of breast cancer after diagnosis of BBD according to whether it was diagnosed in an incident or prevalent screen.
The researchers analysed data from 629,087 women who underwent 2,327,384 screening mammograms between 1995 and 2015, with follow-up until 2017, across seven centres in Catalonia, Asturias and Cantabria. They found that women diagnosed with incident BBD had a 2.67-fold increased chance of developing breast cancer than women with no BBD, while women with prevalent BBD had a 1.87-fold increased risk.
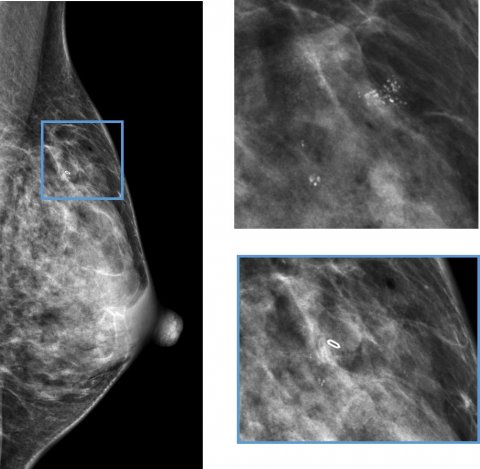
The authors also classified the BBDs as non-proliferative or proliferative, depending on whether or not the breast tissue showed an increase in the growth of certain cells, such as the ductal cells found in ductal hyperplasia, in which there is an overgrowth of cells lining the ducts inside the breast.
The team found that women with proliferative BBD had a 3.28-fold increased chance of breast cancer compared to women with no breast disease, while women with non-proliferative BBD had a 1.96-fold increased risk. ‘We found the highest risk of breast cancer in women with incident, proliferative BBD. They had a nearly four-fold increased risk of breast cancer compared to women with no BBD,’ Román said.
Women with an incident, non-proliferative BBD had a 2.39-fold increased chance of subsequently developing breast cancer compared to women with no BBD; women with prevalent, proliferative BBD had a 2.85-fold increased risk; and women with prevalent, non-proliferative BBD had a 1.63-fold increased risk, the study showed.
A call for personalised screening
Society demands that breast cancer screening, as we know it today, changes and becomes more personalised, integrating all the information that is available
Marta Román
The researchers hope that their findings will be useful in designing personalised breast cancer screening strategies to improve the effectiveness of breast cancer screening. ‘The likelihood that a woman will benefit from screening mammography depends on her risk for developing clinically significant breast cancer in her lifetime. Taking individual risk factors beyond age into account should enable the classification of women into groups at varying risk of breast cancer,’ said Román, whose group is part of MyPebs, an international randomised controlled EU funded trial to investigate whether a risk-based breast cancer screening strategy, based on a clinical risk score, is more effective than stan-dard screening.
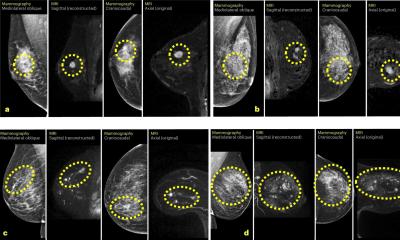
Personalised risk-based screening going beyond the current ‘one-size fits all’ recommendation may increase the effectiveness of breast cancer screening, she believes. ‘Including information from BBD, in addition to other factors, to develop risk-based screening approaches can help with the prediction of whether a woman would develop breast cancer in a defined period.’ Modifying the screening interval, the method of screening - mammogram, ultrasound or MRI - or the age range in which the woman is invited for screening participation could all help improve detection, she suggested.
The new findings should be considered when discussing risk-based personalised screening strategies, to help clinicians understand the different risks associated with benign breast disease and improve the accuracy of breast cancer risk predictions. ‘Society demands that breast cancer screening, as we know it today, changes and becomes more personalised, integrating all the information that is available,’ Román concluded.
Profile:
Dr Marta Román is part of the research group in Epidemiology and Evaluation from Hospital del Mar Medical Research Institute (IMIM). She gained her PhD in Biostatistics at the Universitat de Lleida, and a Masters in Statistics and Operational Research from Universitat Politecnica de Catalunya. Román has extensive experience in epidemiological and clinical research facing national and international projects in the evaluation of breast cancer screening. She is the Director of a PhD thesis dedicated to investigating personalized breast cancer screening strategies. The researcher has published 39 peer review articles on breast cancer screening.
01.12.2020