Image source: Adobe Stock/Mark Kostich
Article • Imaging controversial
MRI breast cancer screening of high-risk women: benefits outweigh drawbacks
Breast MRI is increasingly being used as a primary breast cancer screening exam for young women. It brings benefits in women with dense breasts, who are at an elevated risk of developing breast cancer. The technique is also being ordered as a supplemental screening exam following mammography or breast ultrasound for women of all ages at high risk. But use of breast MRI as a screening tool is controversial. It takes longer for patient set-up and to perform than mammography, may be a scarce imaging resource for radiology departments, and is very expensive compared to the cost of mammography and breast ultrasound exams. However, several recent studies strengthen the argument for breast MRI use as an essential breast cancer screening exam for high-risk women.
Report: Cynthia E. Keen
Women who have extremely dense breasts are four to six times more likely to develop breast cancer than women with mostly fatty breasts. BRCA1 and/or BRCA2 gene mutations are an additional risk factor, putting those affected at an estimated 60% risk of developing breast cancer, compared with 12.5% of women worldwide who have normal BRCA1/2 genes.
Malignant breast tumours of BRCA carriers double in volume very rapidly, increasing their size up to four to five times over 12 months. This rapid tumour size growth, combined with the fact that BRCA1 carriers tend to develop aggressive triple-negative cancers, makes early detection crucial.
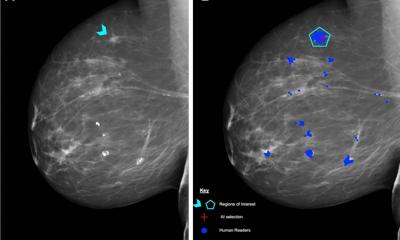
Improving the sensitivity of breast MRI with AI
The sensitivity rate of MRI in detecting early breast cancer in BRCA carriers is as great as 96%, but cancers that look like sub-centimetre lesions with benign appearing features may be overlooked. Researchers at Sheba Medical Center in Ramat Gan, Israel, have developed and clinically tested an artificial intelligence (AI) tool designed to accurately classify enhancing foci seen on breast MR images to help prevent them from being misinterpreted as benign. In its first evaluation test, the AI tool accurately identified more than half of the foci which were initially considered benign but identified as malignant 12 months later.
The researchers had identified 53 BRCA carriers who were diagnosed with breast cancer between 2012 and 2021, and who had had two consecutive breast MRI exams performed at Sheba Medical Center within an 18-month period. They were matched with cancer-free BRCA carrier controls who had been seen at the same clinic with breast MRIs performed in the same time frame.
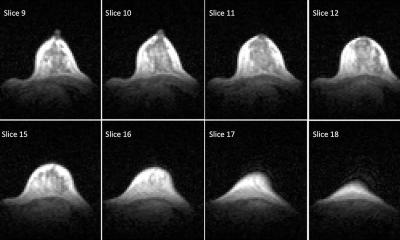
Prior MRIs of both groups were used for analysis, with subsequent diagnostic MRIs serving to identify the tumour area and its delineation. Radiologists manually marked the central slice of the tumour on the sub-dynamic contrast enhanced (DCE) image and used anatomical landmarks to mark the corresponding region in the prior scan. They marked lesions or abnormalities reported in the prior MRI of cancer-free women, or if there were none, marked a prominent enhancing focus. The corresponding region of the subsequent MRI was also marked.
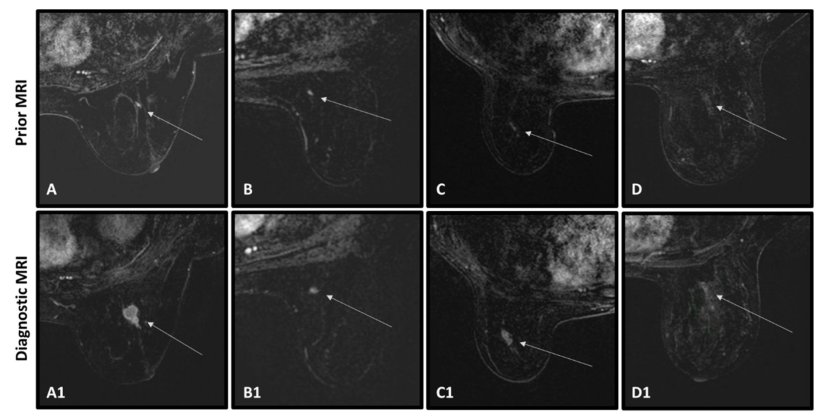
Image source: Anaby et al., Cancers 2023 (CC BY 4.0)
Lead author Debbie Anaby, PhD, head of the Breast Cancer Imaging Laboratory, and colleagues report in Cancers that the AI tool successfully classified 65.6% of cancer cases as cancerous and 88.7% of cancer-free cases as non-cancerous.1 Triple-negative tumours were more frequently successfully classified as cancerous compared with other histological tumour types. Interestingly, in the cancer-free cohort, almost 40% of enhancements detected in the prior scans did not appear in the follow-up MRI.
The researchers are planning a large prospective test and broadening the AI network to an automatic detection of suspicious abnormalities. 'The ability to detect triple-negative breast cancer at such an early stage, while abnormalities are mostly foci with no rim-enhancement, may reduce the clinical burden of the disease,' they write.
Who specifically benefits from breast MRI screening?
The Breast Imaging Clinic at the University of California San Francisco (UCSF) uses both mammography and breast MRI as screening exams for high-risk women. These patients have an annual mammogram, followed by a breast MRI six months later.
'Does breast MRI cancer screening in high-risk women detect early-stage breast cancer?' Lauren Ton, a third-year medical student, asked rhetorically during a scientific session of the Society of Breast Imaging’s (SBI) annual meeting held in late May. 'Yes! Our breast MRI screening detects 99% of cancers before tumour stage 2.’ UCSF recommends that high-risk patients start having mammograms (or breast ultrasound if very young) in their late 20’s or early 30’s. If a family member has had breast cancer, they recommend screening start 10 years before the age the family member was diagnosed.
Ton and colleagues conducted a retrospective study to review the clinicopathologic and imaging outcomes in dynamic-enhanced breast MRIs of patients diagnosed with breast cancer, investigating who specifically benefits from breast MRI screening. The study included all high-risk patients with diagnosed breast cancer who had breast MRI screening between 2012 through 2022, a total of 79 women. They ranged in age from 27 to 71 years. Forty-six percent were pre-menopausal. Most (63%) had heterogenous fibroglandular tissue; only 14% had extremely dense breasts.
BRCA carriers represented 42%, 32% had a personal history of breast cancer, and 11% had a family history. The most commonly detected cancer on breast MRI was invasive ductal carcinoma (55%), with or without ductal carcinoma in situ. Invasive lobular carcinoma represented 6%. The median lesion size was 1.2 cm, with the majority being mass. Fifty-nine percent were detected at tumour stage 1, and 40% at tumour stage in situ. Only 4% of these early-stage breast cancers had axillary lymph node involvement.
'Our findings are comparable to prior studies at other sites,' noted Ton. 'These results support the growing role of screening breast MRI as it enables early breast cancer detection.'
19.02.2024