Image source: Adobe Stock/Valerii Apetroaiei
Article • Additional findings from the MIPA study
Benefits of preoperative breast MRI
Ordering preoperative breast MRI exams of diagnosed breast cancer patients used to be controversial: Did they aid surgical planning better than the combination of mammography and breast ultrasound? Or did their findings cause overtreatment, specifically mastectomy, when breast-conservation surgery would have sufficed? New research has now settled the issue.
Report: Cynthia E. Keen
The real-world analysis of nearly 6,000 patients having surgery as the primary treatment for biopsy-proven breast cancer in 27 centres in Europe, Australia, the United Kingdom, and the United States showed that breast MRIs did not cause overtreatment. And as study data continues to be analysed, it confirms that when breast MRI is ordered, primarily by radiologists and/or breast surgeons, it positively impacts the quality of staging and choice of surgical treatment.
Although data from the MIPA (Multicenter International Prospective Analysis) observational study revealed that 9% more mastectomies were performed than initially planned by surgeons for patients who had a bilateral contrast-enhanced breast MRI, this subgroup of women were at higher risk than those who just had conventional breast imaging. In fact, for a handful of women, breast MRI confirmed the feasibility of breast conservation surgery instead of planned mastectomy.
Screening lead to increased mastectomy rate
Initiated by the European Network for the Assessment of Imaging in Medicine, and funded with an unconditional research grant from Bayer AG, the study recruited 7,245 patients ages 18 to 80. Of these, the data of outcomes for 5,896 were able to be analysed. Based on the recommendations of their physicians and the protocols of their treatment centres, 53.1% had a breast MRI supplementing conventional imaging. In addition to a larger number of women in the breast MRI cohort being younger and pre-menopausal, 17% more had dense breasts, 15% more had tumours larger than 20 cm, and 9% more had a higher rate of invasive lobular histology than the conventional imaging group.
Mastectomy had already been planned for 547 (22.4%) prior to the breast MRI. Post MRI screening, this number increased to 791 women (32.4%), and ultimately 773 were performed based on surgical recommendation. An additional 50 women self-opted to have a mastectomy. By comparison, only 398 (14.4%) of women had planned mastectomies based on conventional imaging findings. This ultimately increased to 432 women, with 19 of this group electing to have a mastectomy instead of recommended breast conservation surgery.
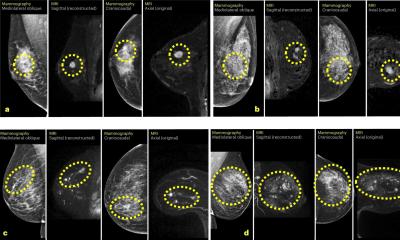
‘MRI did not alter the surgical planning based on conventional imaging in 84.5% of cases,’ wrote principal investigator Prof. Francesco Sardanelli, MD, of the Università degli Studi di Milano, Italy, and co-researchers in European Radiology.1 The surgical planning value of breast MRI is also reflected in reoperation statistics. The MRI group had a significantly lower reoperation rate, at 8.5%, compared to 11.7% in the non-MRI group. By itself, this finding has major implications for the welfare of the patients and medical cost savings as well.
Identifying cancers that otherwise may be missed
In a subsequent analysis published in European Radiology2, Sardanelli and colleagues compared mastectomy rates and reoperation rates among three groups:
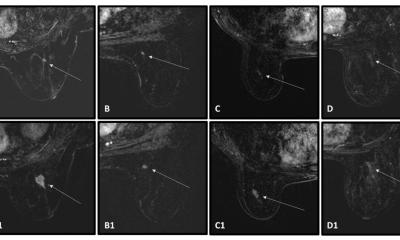
- women for whom breast cancer had already been identified and breast MRI had been ordered for ipsilateral staging, contralateral screening, and surgical intent (79.7%),
- women for whom a diagnostic exam had been ordered, primarily as follow-up to equivocal conventional imaging findings (16.6%),
- and women for whom breast MRI was ordered for breast cancer screening (3.7%).
The screening MRI subgroup proved to be women at the highest risk: younger, with complex cases, larger lesions, the highest rates of small and single-focus cancers, and the highest percentage of familial or personal genetically proven increased risk. The researchers were not surprised that this highest risk subgroup had the highest rate of mastectomies, at 39.5%. By comparison, the rate of mastectomies for the diagnostic group was 24.1%.
Reoperation rates for close or positive margins among the three groups were not significantly different, ranging from 8.2% to 10.5%. However, the difference between the MRI and conventional imaging only groups was. ‘These findings reinforce the fact that breast MRI identifies cancers that may not be seen -- or clearly seen – on mammography and breast ultrasound,’ they commented.
Impact on DCIS in a patient matched analysis
The most recent MIPA data-related study, also published in European Radiology3, evaluates the influence of preoperative breast MRI on mastectomy and reoperation rates in patients with pure unilateral ductal carcinoma in situ (DCIS). Six hundred eighteen patients selected from a group of 1005 with biopsy-confirmed DCIS were equally matched 1:1 to eliminate bias. Three hundred nine had breast MRIs and 309 did not.
The findings again confirmed breast MRI has a positive impact on surgical outcomes. Although the overall mastectomy rate was 23.3% in the group of patients who had breast MRI exams prior to surgery compared to 17.8% in the conventional imaging group, the reoperation rate of the MRI group was dramatically lower. At 23.3%, the reoperation rate of the conventional imaging group was more than double the 10% of the MRI group. ‘The increase in the overall mastectomy rate engendered by preoperative MRI is less than half the corresponding reduction in reoperation rates,’ the authors advise.
References:
- Sardanelli F et al.: Magnetic resonance imaging before breast cancer surgery: results of an observational multicenter international prospective analysis (MIPA); European Radiology 2022
- Cozzi A et al.: Screening and diagnostic breast MRI: how do they impact surgical treatment? Insights from the MIPA study; European Radiology 2023
- Cozzi A et al.: Preoperative breast MRI positively impacts surgical outcomes of needle biopsy-diagnosed pure DCIS: a patient-matched analysis from the MIPA study; European Radiology 2023
28.02.2024