Image source: University of Dundee
News • Prevention of unnecessary emergency admissions
Mobile Stroke Units could reduce pressure on healthcare systems, study finds
A world-leading expert in stroke treatment from the University of Dundee believes that specialised ambulances could prevent hundreds of unnecessary emergency admissions across Scotland each year while ensuring patients receive the best possible care.
Professor Iris Grunwald, Chair of Neuroradiology in the University’s School of Medicine, previously introduced the first Mobile Stroke Unit (MSU) to England, and is keen to see the project replicated north of the border. Professor Grunwald was part of a research team drawn from across Scotland, England and Germany who analysed data comparing outcomes for patients when an MSU responded to a 999 call out as opposed to a conventional ambulance.
MSUs are typically equipped with a CT scanner, point-of-care laboratory, and communications capabilities that enable much faster identification of the stroke type and administration of critical treatments. As well as potentially improving patient outcomes this also prevents unnecessary emergency admissions. The research showed that for patients treated by the MSU, prehospital diagnosis reduced admissions to the emergency department by 86%, either by management at home (46.4%) or by directly transferring patients to the required specialised wards (39.6%).
Even a single MSU could prevent around 600 unnecessary admissions every year, saving 3,000–3,600 bed-days and around £1 million annually
Iris Grunwald
Professor Grunwald says the study demonstrated the feasibility of MSUs and indicated the potential benefits for prehospital treatment and triage decision-making. “NHS Emergency Departments are under immense pressure and so the advantages of MSUs being able to reduce admissions and hospital stays are obvious,” she said. “Time equals brain in instances of stroke so clearly there are also significant benefits to pre-hospital diagnosis that enables better triage decision-making and treatment to begin before the patient even reaches hospital. Someone in the UK experiences a stroke every five minutes. This is a major issue, which takes a significant toll in terms of human and economic costs and in terms of healthcare capacity. The aggregate societal cost of stroke in the UK is estimated at £26 billion per year, including £8.6 billion for NHS and social care.”
The observational study published in the journal Stroke: Vascular and Interventional Neurology examined the outcomes for 500 patients in the East of England area. Half received treatment from an MSU crew and half were conventionally treated. Apart from patients with a dispatch code for stroke, the MSU was also dispatched to those with codes for seizures, falls with head trauma, headache, unconsciousness, infection and pandemic, chest pain, and breathing problems.
Recommended article

Article • Act fast, save lives
Mobile stroke units: when emergency medicine hits the road
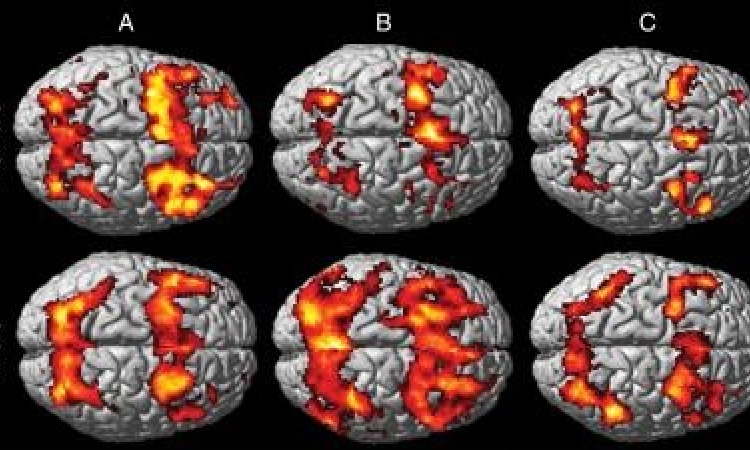
Speed in treatment of ischemic stroke can mean the difference between successful recovery versus permanent disability caused by brain tissue damage or death. Time is of the essence to perform thrombolysis with a tissue plasminogen activate (tPA), a protein that can dissolve blood clots causing the stroke or intra-arterial thrombolytic therapy (IAT) because of large-vessel occlusion.
Professor Grunwald continued, “Questions had been raised about the cost-efficiency of MSUs and how they could be integrated into clinical practice but this study shows clear benefits to their widespread adoption across the country. This research shows that the MSU concept may benefit from equipping them with extended capabilities that make them suitable for dealing with additional emergencies, particularly in non-urban areas.
“If MSUs were supported and funded across Scotland then the impact on patient flow, hospital capacity and emergency care would be transformative, reducing unnecessary admissions, freeing thousands of bed-days, and easing pressure on overwhelmed emergency departments. Even a single MSU could prevent around 600 unnecessary admissions every year, saving 3,000–3,600 bed-days and around £1 million annually. For elderly and frail patients in particular, this means safer care, fewer hospital stays and being triaged to the right place at the right time.”
The study was led by Consultant Neurologist Professor Silke Walter (University of the Saarland), with strategic leadership from Professor Klaus Fassbender, CEO of Intelligent Ambulance Solutions (INTAS) and the inventor of the MSU/ and Hybrid-MSU concepts. The operational work was supported by Professor Grunwald and PhD student Daniel Phillips, a Consultant Paramedic with the East of England Ambulance Service, who evaluated the MSU pathway. Professor Grunwald served as lead for imaging, frequently accompanying the MSU, and later providing teleradiology support, assisted by Drs Saman Perera, Jineesh Thottath (Southend University Hospital) and Avinash Kannodia (NHS Tayside). Also contributing were the East of England Ambulance Service, East Suffolk and North Essex NHS Foundation Trust, and Fred Heddell, Director of the Mobile Stroke Unit Charity, whose long-standing commitment was central to establishing the service evaluated in this study.
Dundee’s position as a global leader in stroke treatment and training was bolstered in October when Professor Grunwald and colleagues took part in the world’s first robotic transatlantic thrombectomy. The event came hours after she performed the first-ever remote thrombectomy on a human cadaver. Using a cutting-edge robot developed by Lithuanian MedTech company Sentante, Professor Grunwald proved that a blood clot could be removed from the brain without a specialist being physically present when she performed the procedure from a remote site within the School of Medicine at Ninewells Hospital. That was followed by the groundbreaking moment when Sentante’s device was used to perform the first transatlantic thrombectomy on a human cadaveric model located at Dundee from Jacksonville, Florida.
Source: University of Dundee
07.01.2026