Measures to contain obesity
The World Health Organisation (WHO) quotes figures that indicate there are over one billion overweight adults spread across the world, as of 2007, with at least 300 million of these defined as clinically obese (as defined by a BMI (body mass index) of 30).
This epidemic of global proportion poses a considerable burden not only on obese individuals, who inevitably share a greater risk for chronic diseases, but also for society, which must cope with the associated healthcare costs. In the US healthcare expenditures related to obesity have been estimated as $100 billion per year.
The main contributors to the epidemic - energy-rich foods high in saturated fats and sugars, combined with a reduction in physical activity – are well known.
America is often viewed as being the frontrunner in obesity; however, since 1980 a three-fold increase in girth has been recorded in people in North America, the UK, Eastern Europe, the Middle East, the Pacific Islands, Australasia and China. Contrary to popular belief, rising obesity rates are not a scourge pertaining to industrialised nations alone – developing countries are showing even faster rates of increased obesity among their population. Most alarming is the trend of obesity in children that is seen across all spectrums of society’s socio-economic groups.
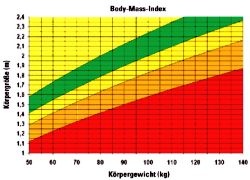
In the US, the percentage of adults defined as obese increased from 15% of the population in 1995 to almost 24% in 2005. About 5% of these are considered extremely – or morbidly – obese (a BMI greater than or equal to 40). The BMI is calculated by the weight in kilograms divided by the height in metres squared. In 2000 it was estimated that 400,000 deaths resulted from obesity and its associated medical conditions. It is believed that in this century the rise in obesity will result in a reduction in the overall life expectancy in affected nations.
A recent article in the New England Journal of Medicine discusses the treatment options available. ‘Bariatric surgical procedures reduce caloric intake by modifying the anatomy of the gastrointestinal tracts,’ according to the review by Dr Eric J DeMaria, of the Duke Weight Loss Surgery Centre at Duke University Medical Centre. Gastrointestinal surgery is recommended in the US for those with a BMI of 40 or above, or 35 with associated medical co-morbidities, such as severe diabetes mellitus, sleep apnoea or heart disease, according to the guidelines developed by the NIH Consensus Development Conference in 1991. The benefit for those with a BMI between 30 and 35 remains unclear.
Surgical operations can be divided into procedures that are either restrictive (gastric stapling or banding) or malabsorbtive (Roux-en-Y gastric bypass). The former consists of creation of a smaller stomach with a narrow opening to prolong the emptying of digested food into the intestines, whereas the latter is created with bypassing of sections of the gut where the absorption of food takes place.
‘The ideal procedure has not been definitively established,’ writes DeMaria in the Journal, citing that in the United States, the Roux-en-Y gastric bypass is the most common operation (open or laparoscopic), while in Europe laparoscopic adjustable gastric banding is more frequently performed. Gastric banding involves wrapping a synthetic band around the stomach that limits its capacity to expand and delays emptying. The role of surgery for those under 18, or above 60 years, has not been established. There have been no randomised clinical trials that compare surgery to medical management of obesity. A 2005 Cochrane review of five studies, including three cohort studies, showed bariatric procedures led to a weight loss of 20-50 kg, compared with a modest weight gain in medically treated patients. A large Swedish prospective trial showed that surgically treated patients followed over two years had significantly greater weight loss than those in the control group.
Defining optimal candidates for surgery remains a challenging. Some morbidly obese individuals may be at risk for complications with surgical intervention. All patients should undergo a comprehensive surgical, medical, psychological and nutritional assessment prior to surgery, according to the journal report.
26.06.2007