Article • AI tool might reduce surgery
Managing cancer-questionable breast lesions
The management of biopsied breast lesions that are diagnosed as abnormal but are not definitively malignant is challenging and controversial. Treatment ranges from diligent follow-up, with imaging and subsequent biopsy, to surgical excision.
Report: Cynthia E. Keen
Researchers at the Medical University of Vienna (Medizinische Universität Wien), Austria, have developed and validated a software algorithm designed to stratify the risk of a breast lesion of uncertain malignant potential, known as a B3 lesion. This could help define the best treatment or follow-up and prevent unnecessary surgeries. Because B3 lesions have an increased risk of malignancy and an increased risk of subsequent development of invasive breast cancer, the practice in many countries is surgical excision. Thus, many women with ultimately benign lesions have unnecessary surgeries.
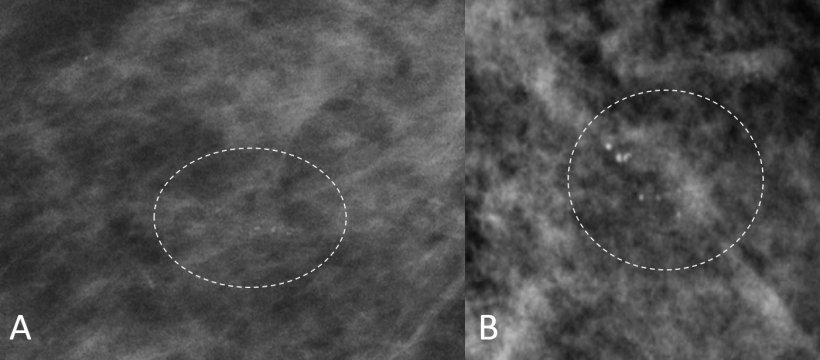
Additionally, with a steadily increasing number of B3 lesions being diagnosed by biopsy, due to improvements in mammography imaging and the worldwide increase in breast cancer screening programs, more precise methods of predicting malignancy are needed. Currently, the risk of missing a malignant component in a B3 lesion ranges from 2-58%. Writing in the February 2021 issue of the European Journal of Radiology, the researchers attribute this wide range to characteristics of the type of biopsy performed (core needle or vacuum-assisted); the lesion type; and diverseness of imaging features, which include microcalcifications, masses, and architectural distortions.
The researchers advise that B3 lesions are identified in 3-11% of stereotactic-guided vacuum-assisted stereotactic biopsies (VABB) performed for suspicious microcalcifications. Their aim was to create a machine learning risk stratification method for VABB diagnosed B3 lesions using a combination of imaging, pathological, and clinical features. The data set used to develop the algorithm included 99 patients with B3 lesions diagnosed and surgically excised at AKH Wien.
The study included a training cohort of 76 patients diagnosed between 2013-2015 and a testing cohort of 23 patients diagnosed in 2016. There were 10 malignant and 66 benign B3 lesions in the training cohort, and six malignant and 17 benign lesions in the testing cohort. The malignant lesions included one invasive ductal carcinoma and 15 ductal carcinomas in situ. Benign lesions in both cohorts included adenosis, fibrocystic changes, and fibrosis, and papillomas in the testing cohort only.
The algorithm utilised clinical information of each patient regarding age at diagnosis, personal history of breast cancer, presence of a concomitant breast cancer, histology of the biopsy and surgical specimens, and diagnostic imaging, which included a BI-RADS classification. Radiologists assessed lesion size, morphology, microcalcification distribution, presence of associated soft-tissue mass, and architectural distortions.

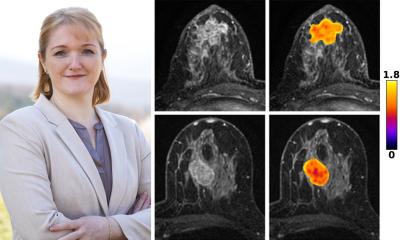
Principal investigator Professor Pascal A T Baltzer MD, and colleagues at the Department of Biomedical Imaging and Image-guided Therapy, reported that the algorithm identified malignancies in more women who had highly suspicious microcalcifications and a concomitant cancer. Their findings suggest that surgery should generally be recommended for microcalcifications with a highly suspicious morphology, and follow-up only with patients who have less suspicious microcalcifications, with round punctate, amorphous, and/or coarse heterogeneous morphology.
If the risk stratification algorithm had been used with these 99 patients, surgery could potentially have been avoided in 25 cases. Baltzer told Healthcare in Europe that the team plans a larger, multi-centric retrospective validation study. They are currently looking for partners. Interested hospital researchers should contact him at pascal.baltzer@meduniwien.ac.at. ‘Our exploratory analysis gives us only a clue about the number of avoidable surgeries,’ he pointed out. ‘This number needs to be substantiated by confirmatory studies. Also, such research could establish whether the missed cancers are indeed biologically minor, or whether we could miss “killer” cancers by the suggested therapeutic de-escalation. We are pursuing this and possibly a prospective multi-centric randomised clinical study.’
Profile:
Pascal Baltzer MD is an associate professor specialising in breast imaging at Medizinische University Wien, where he has worked for the past nine years. Currently he is also Secretary-General of the European Society of Breast Imaging (EUSOBI) and executive board member of the breast imaging working group of the Deutsche Röntgengesellschaft. In July 2020, he was appointed editor-in-chief of the European Journal of Radiology.
04.03.2021