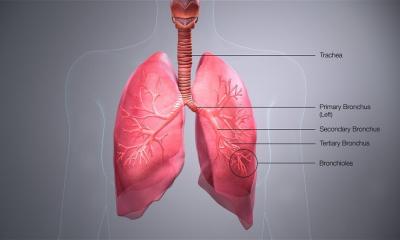
© Axel Kock – stock.adobe.com
News • Reaction to donor organ
Lung transplantation: new findings on life-threatening PLS complication
PLS (Passenger Lymphocyte Syndrome) is a potentially life-threatening risk in lung transplants that has hardly been researched and is often underestimated in clinical practice.
However, the complication occurs more frequently than previously thought, as shown by a recent study at the Department of Transfusion Medicine and Cell Therapy in collaboration with the Department of Thoracic Surgery at MedUni Vienna and University Hospital Vienna. The results, recently published in the American Journal of Respiratory and Critical Care Medicine, not only provide new insights into PLS, but also approaches for early detection and timely treatment.
Our detailed analysis of AB0-mismatched transplants revealed that, depending on the specific blood group combination between donor and recipient, up to 30% of patients developed haemolytic reactions after lung transplantation
Günther Körmöczi
The study is the most extensive research work on this topic to date. Relevant data and parameters from around 1,100 patients who received a lung transplant at the University Hospital Vienna between 2010 and 2021 were analysed. As the results show, PLS occurs significantly more frequently in unequal AB0 settings, i.e. with different blood groups of donor and recipient, than previously assumed. PLS occurs when certain white blood cells (lymphocytes) from the donor's blood trigger haemolysis after transplantation, i.e. destroy the recipient's red blood cells. Patients with PSL have significantly lower haemoglobin levels, are therefore more anaemic and require blood transfusions twice as often as patients without PLS.
"Until now, it was assumed that only a few per cent of patients were affected," reports principal investigator Günther Körmöczi (Department of Transfusion Therapy and Cell Therapy). "However, our detailed analysis of AB0-mismatched transplants revealed that, depending on the specific blood group combination between donor and recipient, up to 30% of patients developed haemolytic reactions after lung transplantation." Blood group A patients who received blood group 0 transplants were particularly frequently affected.
These findings underline the urgency of careful monitoring of important parameters after lung transplantations in the AB0-unmatched setting in order to detect and treat haemolysis at an early stage. The appropriate measures for this (Coombs test, eluate test) were also described in the study. "Immunohaematological monitoring is indicated in AB0-unequal constellations in order to optimally care for patients after lung transplantation and provide them with adapted transfusion therapy," says Körmöczi, emphasising the relevance of the results. The study is a follow up to the diploma thesis by first author Mirjam M. Kohl (Department of Transfusion Medicine and Cell Therapy) under the supervision of Günther Körmöczi and Stefan Schwarz and thus marks a success not only in research but also in teaching at MedUni Vienna.
Source: Medical University of Vienna
05.05.2024