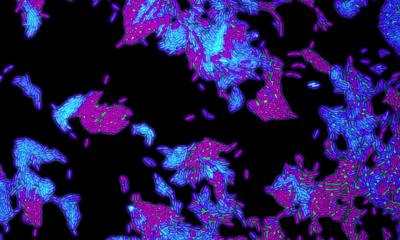
Image source: Adobe Stock/Dr_Microbe
News • Persistence of K. pneumoniae and E. coli
Exploring long-time colonization with resistant enterobacteria
Fighting disease-causing bacteria becomes more difficult when antibiotics stop working. People with pre-existing conditions in particular can carry resistant germs and suffer from repeated infections for years, according to a study by the University and University Hospital of Basel.
Pneumonia, urinary tract infections, sepsis: diseases like these can become fatal without antibiotics. Some bacteria have developed the ability to break down beta-lactam antibiotics like penicillins and cephalosporins, making them ineffective. Once a patient’s body has been colonized by these resistant bacteria, they can persist for a long time, reports Professor Sarah Tschudin Sutter’s research group in the scientific journal Nature Communications.
The team at the Department of Clinical Research of the University of Basel and University Hospital Basel analyzed multiple samples taken from over 70 individuals over a period of ten years. The researchers looked at a much longer period of time than previous studies and focused on older people with pre-existing conditions. Their key question: whether and how resistant Klebsiella pneumoniae and Escherichia coli bacteria in the body change over this long period and how they differ in various parts of the body.
These patients not only repeatedly become ill themselves, they also act as a source of infection for other people – a reservoir for these pathogens
Lisandra Aguilar Bultet
DNA analysis indicates that the bacteria initially adapt quite quickly to the conditions in the colonized parts of the body, but undergo few genetic changes thereafter. The resistant bacteria could still be detected in the patients up to nine years later. “These patients not only repeatedly become ill themselves, they also act as a source of infection for other people – a reservoir for these pathogens,” says Dr. Lisandra Aguilar Bultet, the study’s lead author. “This is crucial information for choosing a treatment,” explains Professor Tschudin Sutter. If someone has previously been infected with resistant bacteria and later requires another course of treatment because of a new infection, there is a risk that standard antibiotics will again fail to work.
In addition, the researchers found that in some patients, bacterial strains of the same species, as well as of different species (specifically, Klebsiella pneumoniae and Escherichia coli), share identical genetic mechanisms of resistance through what are known as mobile genetic elements (such as plasmids). The most likely explanation is that they have transmitted these elements to each other.
Recommended article

Article • Bacterial defense mechanism
Antibiotic resistance: a global threat to healthcare
Antimicrobial resistance (AMR) is becoming more prevalent around the world, constituting a serious threat to public health. When bacteria acquire resistance against antibiotics, common medical procedures – for example, in surgery – become impossible due to the high infection risk. Keep reading to find out about AMR research, development of new antibiotics and antibiotic alternatives.
Hospitals use special protective measures if a patient has been infected with resistant bacteria in the past. In everyday life, however, it is difficult to reduce the risk of pathogen transmission.
These findings about the bacterial genetic diversity expected to develop in individual patients over time are a valuable basis for future studies to analyze factors found in both bacteria and patients that correlate with duration of colonization and progression from colonization to infection.
Source: University of Basel
05.02.2024