Article • Incidental findings
Liver lesions are most often benign
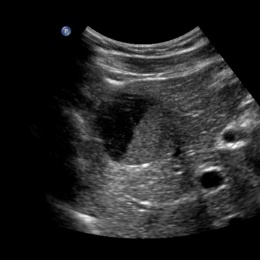
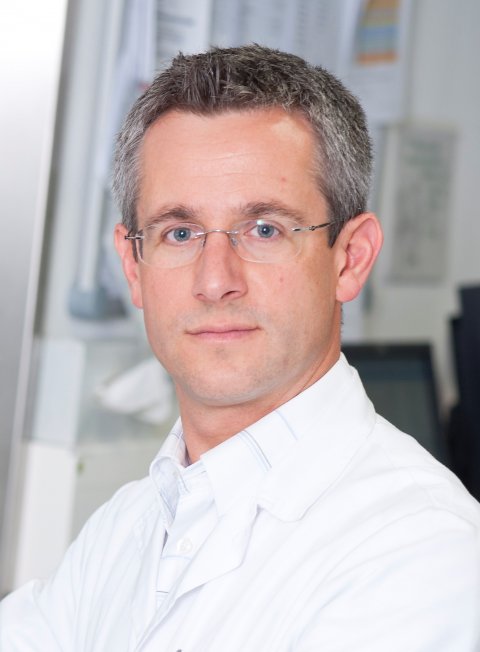
At least 60% of liver lesions can be characterised purely by ultrasound. Screening and examinations of supposedly healthy patients often result in an accidental discovery of liver lesions. According to Dr Antonius Schuster MD MBA, Head of the Department of Radiology at the LKH Bregenz, (Vorarlberg).
Report: Michael Krassnitzer
‘The prevalence of such changes is around 20% of patients examined’. Depending on a patient’s age, around 70% of these liver lesions are benign and 30% malignant. Even in tumour patients between a quarter and half of all changes diagnosed in the liver are benign. ‘If you find a liver lesion the probability is high that it is a benign change,’ he said.
What happens next depends on morphology ultrasound and the clinical context. The course of action for tumour patients is more clearly governed than the treatment of incidental liver lesions in healthy patients. The examiner is on his own when it comes to deciding the next steps, because there are no recommendations from specialist medical societies and associations on how to proceed, Dr Schuster pointed out.
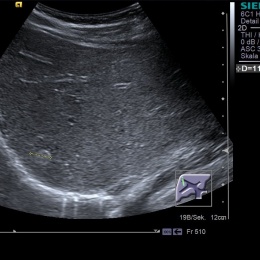
To ensure patients do not become unnecessarily concerned, and to avoid further expensive examinations, or possible complications that can occur in the course of these examinations, it is important that as many as possible benign changes are also diagnosed. At least 60% of the lesions can be characterised purely with ultrasound. Those that cannot be safely diagnosed in this way should be examined with the help of contrast-enhanced ultrasound (CEUS), ideally during the same examination. ‘Contrast enhanced ultrasound is a tool that can be used to diagnose and differentiate changes between benign and malignant with extremely high certainty,’ Schuster emphasised: ‘However, how much certainty depends on the experience and expertise of the examiner.’
In cases where a CEUS exam does not lead to a clear diagnosis, or when it is not available, the next step would be a scan via CT, MRI, scintigraphy and aspiration as a last resort. Schuster: ‘To avoid over-diagnosis, one should check a benign incidental diagnosis after three months and only proceed with further evaluation in case of a change to the initial findings.’
However, in his lecture he will give recommendations based on clinical practice. Briefly summarised: In cases of unclear ultrasound diagnosis, please carry out CEUS or a control scan; after that, only when there is still uncertainty should a CT or MRI scan be performed. He offers a further tip: ‘Patients with a tumour anamnesis can be given a CT scan straightaway, because in any case the oncologist will be interested to see where else metastases might be.’ This is where ultrasound has its limitations – it cannot be used to scan the lungs or the bones.
Profile:
Antonius Schuster MD MBA heads the Department for Radiology at the regional hospital in LKH Bregenz. After gaining his medical degree and specialist training at Innsbruck’s University Hospital and being a specialist registrar there, in 2002 he moved to Feldkirch Hospital, where he became a specialist in 2005, and was then appointed Senior Consultant in the Department of Radiology. Dr Schuster is a member of the Austrian Medical Examination Board for Radiology and has published 22 original papers as primary, senior and co-author. In his work and research his focus lies on interventional radiology, multimodal oncological imaging, contrast-enhanced and musculoskeletal ultrasound as well as cardiovascular imaging (cardiac CT, cardiac MRI).
10.11.2014